Late Local Urticaria as a Long-term Sequela of Allergen-Specific Immunotherapy
Article information
Abstract
Local reaction to allergen-specific immunotherapy (SIT) usually appears within 30 minutes, but cases with exercise-induced urticaria at the SIT site 2–3 weeks after the last allergen injection have been reported. A 28-year-old man was treated with house dust mite-SIT for 5 years, due to asthma when he was an 11-year-old boy. On a treadmill exercise test for 50 minutes, erythema, swelling, and pruritus occurred at the SIT site, which lasted for one hour. There was no evidence of complement activation, and the skin biopsy specimens showed no apparent difference between the lesion and normal sites in the distribution of inflammatory cells and in mast cell degranulation. However, the morphine, but not the histamine, skin test responses were increased after the exercise. There must be a remaining long-term sequela of the SIT, including an increased releasability of mast cells, even after more than 10 years.
INTRODUCTION
Local reaction to allergen-specific immunotherapy (SIT) usually appears within 30 minutes. However, allergens can induce not only an immediate hypersensitivity reaction, but also allergic inflammation or other long-term sequelae that cause episodic symptoms precipitated by nonspecific stimuli. This phenomenon might also occur at the SIT site. Several reports have demonstrated such SIT-associated reactions. Rotne1) reported two cases that developed local or systemic reactions in connection with physical exercise, and Garcia, et al.2) showed two cases of localized cold urticaria. Here, a case that developed local cholinergic urticaria at the SIT site, more than ten years after the completion of five years of SIT, is reported.
CASE REPORT
A 28-year-old man had suffered from asthma and allergic rhinitis for more than 20 years. When he was an 11-year-old boy, he sought therapy for his diseases, at Chonnam National University Hospital, and was treated with house dust mite-SIT for five years, without adverse reactions (Bencard, Brantford, UK). His allergic diseases went into remission for about two years after the last injection of SIT. He subsequently used bronchodilators as needed, but in December 2002, revisited the hospital due to dyspnea [forced expiratory volume in one second (FEV1): 64% of predicted value]. At this time, he complained of frequently occurring itching eruptions, which appeared on his left upper arm at the former injection sites when he exercised.
One month after a short course of anti-asthma therapy and withholding all medications for more than one week, he underwent a six-minute free-running test. One minute after the test, the FEV1 had decreased to 1.83 L (44% of predicted value) from the baseline (3.0 L, 72%), but urticaria was not observed. The patient said that urticaria occurred only when he exercised for a period much longer than the six-minute test. Two days later, he underwent a treadmill exercise test for 50 minutes. Blood sample analyses and skin tests before and 20 minutes after the exercise, and skin biopsies after the exercise were performed.
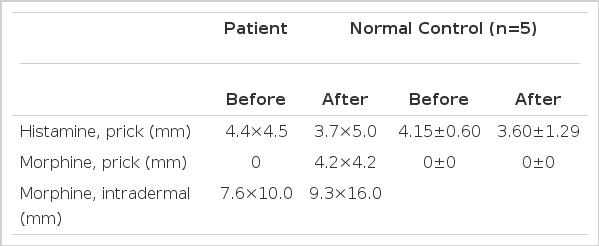
A methacholine intradermal test (0.01 mg in 0.1 mL) was negative before the exercise. Erythema, swelling, and pruritus occurred at the SIT site 30 minutes after the exercise test started, and lasted for one hour after the completion of the test (Figure 1). There was no evidence of complement activation. The biopsy specimens showed no apparent difference between the lesion and the normal sites in the distribution of inflammatory cells and in mast cell degranulation under light and electron microscopic examinations. However, the morphine, but not the histamine, skin test responses were increased after the exercise (Table 1). The control subjects (n=5, 20.6±0.9 year-old men) showed no significant difference in the skin test responses before and after exercise.
Pruritic erythema and swelling of the skin of the upper arm, the former specific immunotherapy site, developed 30 minutes after the exercise test started.
DISCUSSION
Reports have described localized2, 3) or generalized4) cases of cold urticaria during SIT. Rotne1) reported cases with exercise-induced urticaria at the SIT site two to three weeks after the last allergen injection. These cases developed urticaria during SIT. In our case, however, more than ten years had passed since the patient completed his five-year SIT schedule. This suggests a long-term sequela for SIT.
It is well known that cholinergic urticaria appears associated with exercise, hot showers, and sweating. The local form of cholinergic urticaria and its association with histamine release has been demonstrated5). Even though about one-third of patients with cholinergic urticaria show a positive response to a methacholine skin test (immediate hypersensitivity to cholinergic mediators), the exact pathophysiologic mechanisms have not been elucidated.
A possible explanation for the complicated phenomena comprised of local urticaria or generalized allergic reactions to stimuli, such as cold, heat, and exercise, following SIT has been proposed. Allergens can induce allergic inflammation, or other long-term sequelae, which make lesion sites susceptible to various stimuli responses. It has been shown that atopic subjects have an increased releasability of mast cells in response to nonimmunologic stimulation, such as morphine6). Although the case in the present study showed no evidence of mast cell degranulation on electron microscopic examinations, he showed a greater skin response to morphine than a normal control. Moreover, his skin response to morphine, but not to histamine, was increased after the exercise challenge. It is unclear how exercise primes an increase in the histamine release from mast cells in response to morphine. However, late recall urticaria has been observed after injection of allergen in the arm that had not received allergen administration during the SIT7). In addition, there have been reports of strong local urticaria at the sites of methacholine testing, but only following an exercise test in some patients with cholinergic urticaria8), and a marked increase in the wheal response to compound 48/80 (a cutaneous mast cell degranulating agent), but not to histamine, after a combination of food and exercise challenges in patients with food-associated exercise-induced urticaria-angioedema9). These observations corroborate the results of our study in several regards.
Taken together, nonspecific stimuli, such as cold, heat, exercise, and morphine, may precipitate the occurrence of allergic symptoms, including recall urticaria at the SIT site, even after a long time period, and especially during the exacerbation period of atopic diseases. Allergen-induced long-term sequelae, including an increased releasability of mast cells, may make the lesion sites more susceptible to various stimuli responses.