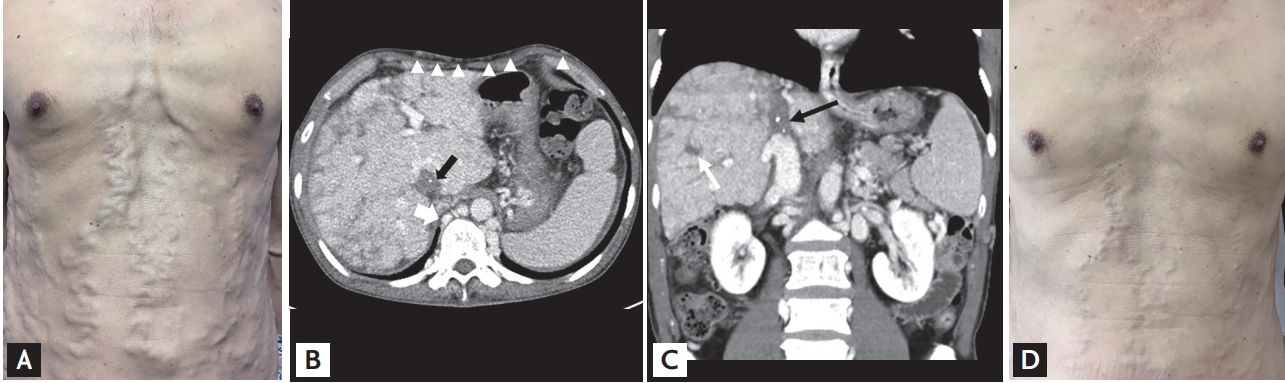
A 70-year-old man without any underlying disease was admitted to our hospital complaining of abdominal discomfort for 3 months. He denied alcohol consumption but was a current smoker with 20 pack-year history of smoking. His physical examination revealed grossly engorged and tortuous veins of the abdominal wall (Fig. 1A) and mild scleral icterus. His laboratory findings revealed the following: total bilirubin level of 3.68 mg/dL, prothrombin time of 14.8 seconds, and platelet count of 96,000/┬ĄL. Abdominal computed tomography demonstrated a massive thrombus in the inferior vena cava (IVC) with prominent proliferation of collateral vessels and subcutaneous collaterals (Fig. 1B and 1C). The liver was enhanced heterogeneously with multiple regenerative nodules. Further investigations were completed to detect the cause of thrombosis of the IVC, but no cause was found. Thus, a diagnosis of idiopathic Budd-Chiari syndrome (BCS) with thrombosis of the IVC was established. The patient received anticoagulation therapy with rivaroxaban. The abdominal wall varices had improved markedly 6 months after therapy (Fig. 1D).
BCS is a rare disease characterized by impaired hepatic venous outflow at the level of the hepatic venules, large hepatic veins, IVC, or right atrium, regardless of the cause of obstruction. Clinical manifestations may be diverse, ranging from asymptomatic to acute hepatic failure, depending on the extent and rapidity of hepatic vein occlusion and on whether venous collateral circulation has developed to decompress the liver sinusoids. Up to 20% of cases diagnosed as BSC are idiopathic. All patients with BCS are recommended to undergo anticoagulation therapy based on the consensus of expert opinions. Other therapeutic options include endovascular treatment (local thrombolysis, stenting, and angioplasty), placement of a transjugular portosystemic shunt, or orthotopic liver transplantation in selected patients. According to our experience, when abdominal wall varices are observed, BCS may be considered in the differential diagnosis.
Written informed consent were obtained.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print





