To the Editor,
Behcet's disease (BD) is an inflammatory disorder of unknown cause characterized by recurrent oral aphthous ulcers, genital ulcers, uveitis, and skin lesions [1]. It may also involve the gastrointestinal tract, central nervous system, and cardiovascular system. Cardiac involvement in BD is uncommon; it has been reported in only 1% to 6% of patients with BD [2]. Cardiac abnormalities in patients with BD include pericarditis, myocarditis, endocarditis with valvular regurgitation, intracardiac thrombosis, endomyocardial fibrosis, coronary arteritis with or without myocardial infarction, and aneurysms of the coronary arteries or sinus of Valsalva. We herein report a rare case involving a cardiovascular manifestation of BD, which presented as acute cerebral infarction due to an intracardiac thrombus within the cavity of the interventricular septum (IVS).
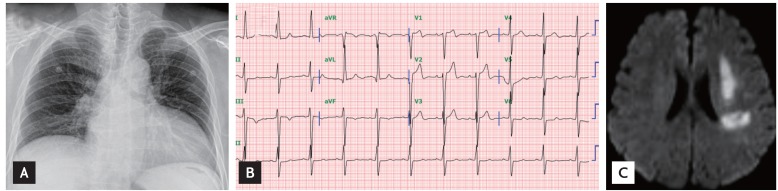
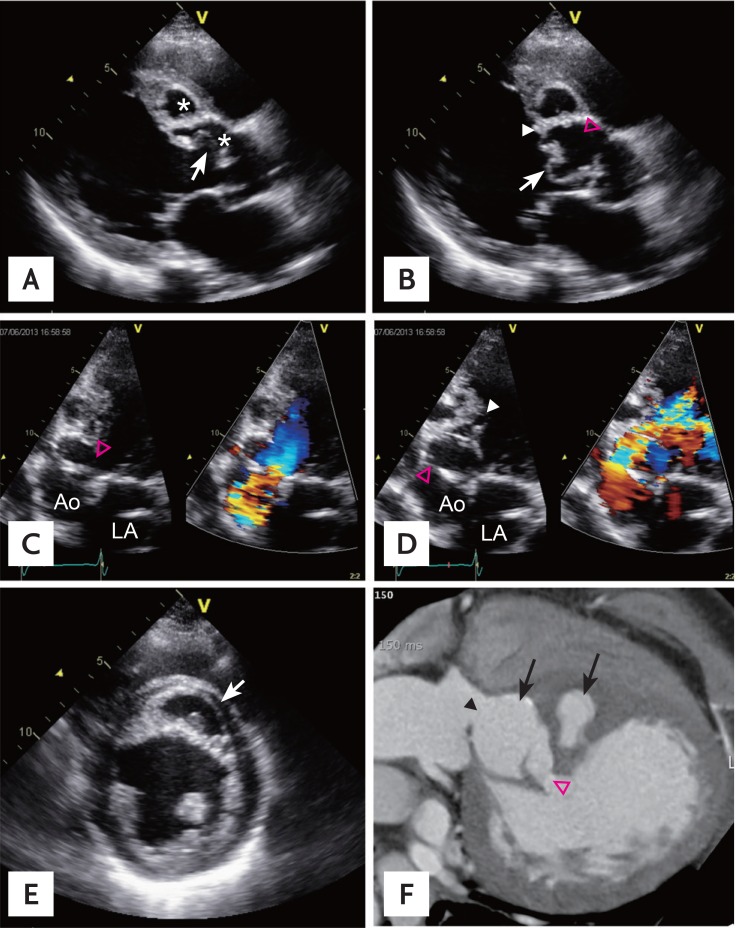
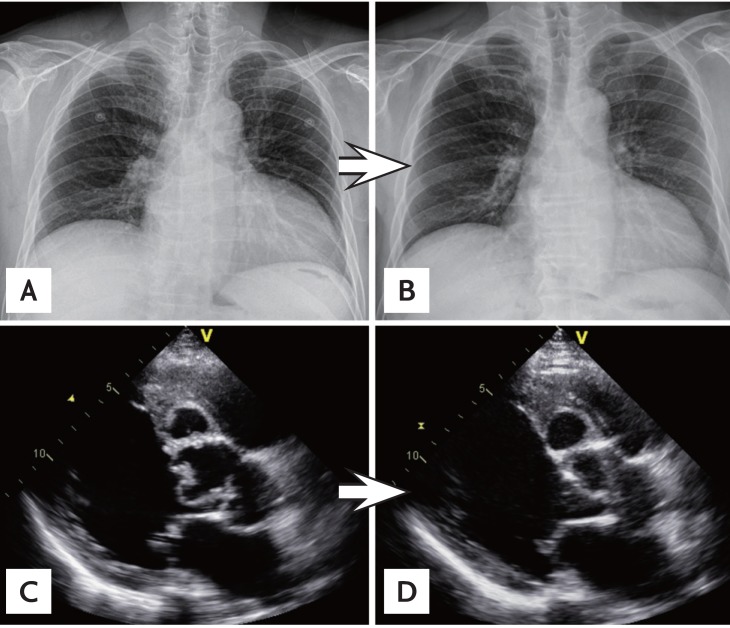
A 58-year-old male presented to our emergency department with a 10-hour history of dysarthria. He had undergone surgery for extrahepatic cholangiocarcinoma 7 months previously and had completed adjuvant chemotherapy until the last month at another hospital. At presentation, his blood pressure was 130/50 mmHg and his heart rate was 66 beats per minute. On physical examination, he showed dysarthria and facial palsy as well as a systolic and diastolic murmur. A chest radiograph demonstrated cardiomegaly, and an electrocardiogram showed a normal sinus rhythm with hypertrophy of the left ventricle (LV) (Fig. 1A and 1B). Laboratory tests revealed anemia (hemoglobin, 7.9 g/dL; reference range, 11.7 to 17.1) and an elevated C-reactive protein level (73 mg/L; reference range, 0 to 5), but both the white blood cell count and percentage of neutrophils were normal. Magnetic resonance imaging of the brain was immediately performed and showed acute ischemic infarction (Fig. 1C), and the patient was admitted to the stroke unit. On the 5th day after admission, transthoracic echocardiographic examination (TTE) was performed for cardiac evaluation and showed a perforation of the sinus of Valsalva and a dissection involving the IVS (Fig. 2A-2D). The dissection of the IVS resulted in the formation of two cavities in the basal and mid-IVS (Fig. 2A). The larger basal cavity communicated with the aorta and LV through a perforation in the aortic root and another perforation in the basal IVS into the cavity of the LV (Fig. 2B). These unusual structural changes caused significant aortic regurgitation through the perforations. The LV cavity collapsed during systole because of the redundant dissecting flap of the IVS (Fig. 2A), allowing systolic outflow into the aortic valve (Fig. 2C). During diastole, the redundant dissecting flap bulged into the LV cavity (Fig. 2B) and regurgitant flow was observed from the aorta into the LV through the perforations (Fig. 2D). The regurgitant volume seemed to be compatible with severe aortic regurgitation based on the color Doppler image (Supplemental Video 1A, available online at http://www.kjim.org/) and diastolic reversal of flow in the proximal descending aorta. The LV chamber size was also increased (LV end-diastolic dimension, 69 mm; LV end-systolic dimension, 51 mm). On the other hand, in the short-axis view, a small round thrombus was observed within the IVS cavity (Fig. 2E). Cardiac computed tomography also demonstrated the abnormal structure of the aortic root and the IVS, with findings similar to those of TTE (Fig. 2F). After cardiac evaluation, we obtained a detailed history, which revealed a > 30-year history of recurrent oral and genital ulcers. Based on a subsequent positive pathergy test, the patient was diagnosed with BD. His cardiac and aortic abnormalities were revealed to be cardiovascular manifestations of BD after excluding other possible etiologies, such as bacterial endocarditis, based on negative blood culture tests. When we reviewed his previous TTE performed 7 months previously at another hospital (before his abdominal surgery), we identified a similar but less severe cardiac lesion than that observed on the current TTE. Based on the previous TTE, his cardiac condition was considered to be relatively chronic. We started anticoagulation therapy for the intracardiac thrombus, immunosuppressive therapy (prednisolone, azathioprine, and colchicine) for the BD, and medication for heart failure. We also planned surgical treatment of his cardiac lesion. However, the patient and his family refused cardiac surgery at that point. Therefore, he was treated medically. He has been followed up for 1 year without any cardiac events. Fig. 3 shows his follow-up chest radiography and echocardiography images 6 months after diagnosis. His initial cardiomegaly had slightly decreased at the follow-up examination (Fig. 3A and 3B). Follow-up TTE showed that the cavity of the IVS had become slightly smaller (Fig. 3C and 3D) and that the aortic regurgitant flow had decreased (Supplementary Video 1, available online at http://www.kjim.org/). Finally, his cardiac dimensions had slightly decreased (LV end-diastolic dimension, 65 mm; LV end-systolic dimension, 48 mm).
BD is a multisystemic vasculitis involving both veins and arteries of all sizes. It is especially common among the East Asian and Mediterranean populations. Because BD has no pathognomonic symptoms or laboratory findings, the diagnosis is based on the criteria proposed by the International Study Group for BD in 1990. According to these criteria, we diagnosed BD in the present case based on the patient's recurrent oral and genital ulceration and positive pathergy test. His cardiac lesions, including perforation of the sinus of Valsalva, dissection of the IVS, and intracardiac thrombus, could not be explained by any etiology other than BD. Bacterial endocarditis is a differential diagnosis for cardiac BD. Based on the repeated negative blood culture results and absence of fever, we excluded bacterial endocarditis in this case. Additionally, the cardiac lesion showed a morphology similar to that of two previously reported cases of cardiac BD [3,4]. Both previous cases showed perforation of the sinus of Valsalva and dissection of the IVS, as observed in our case. Interestingly, our patient also showed an intracardiac thrombus, one of the cardiac manifestations of BD, and had ischemic stroke. The two previously described patients were successfully treated with cardiac surgery. However, their long-term follow-up outcomes were not reported. A case involving a similar morphological abnormality as in our case was recently reported in Korea [5]. In that case, however, neither the cause of the cardiac lesion nor whether the patient had BD was reported. The outcome of BD with cardiovascular involvement is poor [3]. Surgical treatment of cardiovascular complications of BD is associated with a high risk of postoperative morbidity due to valve detachment or pseudoaneurysm formation at the anastomotic sites. The present patient was treated medically without surgery, and no cardiac events were noted for 1 year; additionally, an improved cardiac lesion was observed on follow-up examination. To the best of our knowledge, this is the first report of medical treatment of perforation of the sinus of Valsalva and dissection of the IVS in a patient with BD along with presentation of the 1-year follow-up results.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print





