 |
 |
| Korean J Intern Med > Volume 29(6); 2014 > Article |
|
Abstract
The Korea Acute Myocardial Infarction Registry (KAMIR) was the first nationwide registry data collection designed to track outcomes of patients with acute myocardial infarction (AMI). These studies reflect the current therapeutic approaches and management for AMI in Korea. The results of KAMIR could help clinicians to predict the prognosis of their patients and identify better diagnostic and treatment tools to improve the quality of care. The KAMIR score was proposed to be a predictor of the prognosis of AMI patients. Triple antiplatelet therapy, consisting of aspirin, clopidogrel and cilostazol, was effective at preventing major adverse clinical outcomes. Drug-eluting stents were effective and safe in AMI patients with no increased risk of stent thrombosis. Statin therapy was effective in Korean AMI patients, including those with very low levels of low density cholesterol. The present review summarizes the 10-year scientific achievements of KAMIR from admission to outpatient care during long-term clinical follow-up.
The Korea Acute Myocardial Infarction Registry (KAMIR) was the first nationwide, population-based, multicenter registry, and was launched in November 2005. The ethics committee at each participating institution approved the study protocol. Informed consent was obtained from each patient. Trained study coordinators at each participating institution collected the data using a standardized format. Standardized definitions of all variables were determined by the steering committee board of KAMIR. Data were submitted via password-protected web-based electronic case report forms.
KAMIR is an ongoing registry that covers the complete spectrum of acute myocardial infarction (AMI), including long-term clinical follow-up. The registry included 55 representative centers, and contained data from ~52,000 patients over a 10-year period. A total of 122 publications have used KAMIR data, including 103 articles in Science Citation Index journals. The most important aspect of this great accomplishment is that the clinical data have been made available to all participating centers without limitations. The present review focuses on the results of publications regarding AMI, from admission to the outpatient department, over a 1-year follow-up. The publications were divided into three categories based on predictors of prognosis, treatment, and special patient groups.
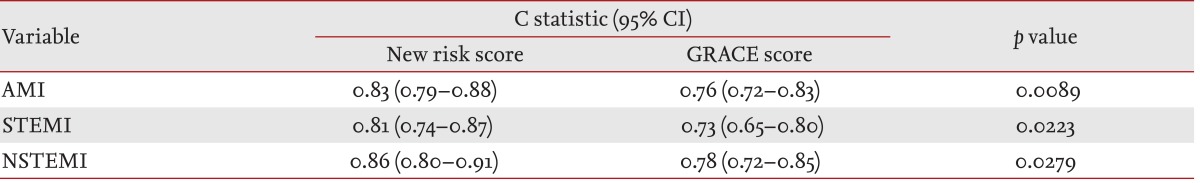
Risk assessment at the time of admission and discharge is important for deciding treatment strategy and postdischarge management. Thrombolysis in myocardial infarction (TIMI) risk score and the Global Registry of Acute Coronary Event (GRACE) risk models are examples of tools for risk stratification. However, these models were developed and validated from the late 1990s to the early 2000s. The rate of percutaneous coronary intervention (PCI) and use of clopidogrel was only 30% during that period, whereas these treatments are used in approximately 90% of patients currently. Furthermore, previous models did not consider risk factors such as: admission hyperglycemia, the presence of stroke or peripheral artery disease, and left ventricular systolic function. Most importantly, TIMI and GRACE risk scores focused predominantly on western AMI patients. KAMIR score was developed for admission and postdischarge risk prediction over a 1-year period [1,2]. The KAMIR score is composed of six independent variables related to 1-year mortality: age, Killip class, serum creatinine, no in-hospital PCI, left ventricular ejection fraction, and admission glucose (Fig. 1). The KAMIR score exhibited significant differences in prediction accuracy compared with the GRACE model in a validation cohort (Table 1). The CHA2DS2-VASc scoring system was also useful for risk stratification in patients with AMI, irrespective of atrial fibrillation [3,4].
Hypertensive AMI patients had worse outcomes, but antecedent hypertension was not associated with 1-year mortality [5,6]. Patients with prior cerebrovascular disease (CVD) presented more frequently with non-ST segment elevation myocardial infarction (NSTEMI), were less likely to receive reperfusion therapy, and had worse clinical outcomes compared with patients without a history of CVD [7]. A family history of coronary artery disease was an independent prognostic factor, particularly in patients with low risk profiles and female gender [8]. Surprisingly, both smoking and obesity were risk factors for AMI development, but were associated with decreased mortality rates after AMI. These phenomena were also observed in KAMIR [9,10,11,12].
A disparity between ST-segment elevation myocardial infarction (STEMI) and NSTEMI was observed [13,14]. Patients admitted during off-hours had a longer waiting time until their procedure, and received less PCI compared with on-hours visitors. In contrast, there was no clinical impact in patients with NSTEMI [15]. However, in-hospital mortality was increased in patients with STEMI [16]. An additional report showed that the time delay in STEMI was not associated with in-hospital mortality [17]. In addition to treatment delay, the incidence of AMI varied according to the season and month. Meteorological parameters, including air temperature, humidity, and sunshine duration, had a significant influence on the occurrence of AMI, particularly in young and female patients [18].
Painless AMI occurred in individuals that were older, female or non-smokers, or had diabetes mellitus (DM) or renal failure; these patients had worse outcomes [19,20]. N-terminal pro-B-type natriuretic peptide levels were associated with short-term mortality in patients with primary PCI [21]. Renal dysfunction and C-reactive protein also had prognostic effects for AMI [22,23,24].
Unprotected left main artery-related AMI resulted in fatal in-hospital outcome, even in cases with non-culprit lesions [25,26]. However, no significant differences were detected in hospital survivors during long-term follow-up [27,28]. Patients with NSTEMI and total occluded infarct-related artery had a worse outcome than did those with non-occluded NSTEMI [29]. Left circumflex artery-related AMI was associated with reduced ST-segment elevation and treatment-delay [30]. Interestingly, AMI patients with non-significant stenosis in a coronary angiogram had a similar outcome as patients with one- or two-vessel disease [31].
Medical treatment is an essential option and interventional management in patients with AMI. Intensive medical treatment might improve the in-hospital outcome of patients who did not undergo PCI [32]. β-Blocker treatment reduced the long-term mortality in patients with MI and preserved systolic function during PCI [33]. Insurmountable angiotensin II receptor blockers (ARB) were more effective than ARB in AMI [34]. Dual blockage of the renin-angiotensin system using angiotensin-converting enzyme inhibitor and ARB could increase the risk of adverse outcomes in severe renal dysfunction patients, without eliciting any clinical benefits [35]. Trimetazidine and nicorandil were not class I drugs in AMI. Additive effects of the use of these drugs have been reported; however, additional studies are needed [36,37].
The optimal loading dose of clopidogrel in Asian patients has not been investigated fully. Data in the KAMIR revealed that the standard loading dose clopidogrel group had similar clinical results compared with the double loading dose group before PCI [38,39]. Low-molecular-weight heparin was associated with a better clinical outcome than unfractionated heparin in patients with AMI [40,41,42].
Early elective PCI after successful thrombolytic therapy for STEMI remains a controversial recommendation. Patients who underwent PCI within 48 hours of thrombolytic therapy had a long-term clinical benefit compared with those who underwent PCI later [43]. In early latecomer AMI (12 to 72 hours after symptom onset), PCI was associated with a significant improvement in the 12-month clinical outcome [44]. The optimal revascularization strategy in AMI patients, culprit-only or total revascularization, remains unclear. KAMIR reported different results between patients with STEMI or NSTEMI. In NSTEMI, multivessel PCI yielded a better clinical outcome without increasing in-stent restenosis and the progression of diseased vessels (hazard ratio [HR], 0.658; 95% confidence interval [CI], 0.45 to 0.96; p = 0.031) [45]. However, multivessel PCI increased target lesion revascularization without any clinical benefit in STEMI [46].
Drug-eluting stents (DESs) were implanted in > 90% of AMI patients in Korea (Table 2) [47]. DESs were superior in terms of promoting target lesion revascularization and had similar safety outcomes compared with bare metal stents (BMSs) in patients with large coronary artery and renal insufficiency [48,49]. Among the DESs, sirolimus-eluting stents (SESs) and everolimus-eluting stents were similar or better than paclitaxel-eluting stents and early-type zotarolimus-eluting stents in terms of target lesion failure [50,51,52,53,54,55]. Intravascular ultrasound-guided PCI did not reduce restenosis and thrombosis in AMI patients [56]. Thrombus aspiration did not improve the clinical outcome of overall patients who underwent primary PCI. In a subgroup analysis, left anterior descending artery occlusion patients had a better prognosis when thrombus aspiration was performed. In addition, the use of a glycoprotein IIb/IIIa inhibitor had a synergistic effect with thrombus aspiration [57].
The optimal medical therapy after discharge was prescribed at suboptimal rates, particularly in high-risk AMI patients [58,59]. Early and continuous statin therapy improved the prognosis after AMI [60]. Lifesaving medications, including lipid-lowering drugs, were underused in patients with lower low-density lipoprotein cholesterol (LDL-C) levels. More intensive treatments, including lipid-lowering therapy, for AMI in patients with lower LDL-C level might improve clinical outcomes [61]. Statin therapy in patients with LDL-C levels < 70 mg/dL was also associated with improved clinical outcomes (Fig. 2) [62]. Stent thrombosis could be reduced by statins in AMI patients with levels of high C-reactive protein [63]. Statins were also effective in patients with renal dysfunction [64].
Dual antiplatelet therapy (DAPT) using aspirin combined with thienopyridine agents such as clopidogrel has become a mainstay of secondary prevention strategies after AMI. Clopidogrel has complimentary effects with aspirin, and reduces adverse cardiac events, including stent thrombosis, compared with aspirin plus warfarin or aspirin alone. However, clopidogrel is a prodrug that requires activation by specific hepatic cytochrome p450 enzymes. This two-step activation process is susceptible to interference by genetic polymorphisms, which can lead to the phenomenon of clopidogrel "nonresponders." Use of an increased dose, addition of other drugs, and development of more potent drugs have been attempted to overcome these shortcomings. In KAMIR, triple antiantiplatelet therapy (TAPT; DAPT + cilostazol) resulted in significantly lower incidences of cardiac death (HR, 0.52; 95% CI, 0.32 to 0.84; p = 0.007), total death (HR, 0.60; 95% CI, 0.41 to 0.89; p = 0.010), and total major adverse cardiac events (HR, 0.74; 95% CI, 0.58 to 0.95; p = 0.019) compared with DAPT in patients with STEMI at the 8-month follow-up [65]. However, the no-reflow phenomenon is a poor prognostic factor for in-hospital mortality after primary PCI [66]. Nevertheless, TAPT was superior to DAPT in patients with AMI who had no-reflow during PCI [67].
There were no gender differences in the initial treatment of AMI. However, the first KAMIR study showed that the success rate of PCI in NSTEMI was lower and the incidence of adverse events after 1 month was higher in females [68]. However, subsequent studies revealed that female gender itself was not an independent risk factor for in-hospital mortality in a multivariate analysis [69,70]. The gender effects might be age-dependent, or due to the presence of more comorbidities and severe hemodynamic conditions at presentation [71].
Generally, DM was a poor prognostic factor for mid-term (1 month to 1 year) clinical outcomes, but not for the short-term prognosis (~1 month) in AMI patients [72,73]. Glucose levels at the time of admission were a prognostic factor for short-term clinical outcomes in the KAMIR. Hyperglycemia at admission was an independent predictor of 1-month mortality in non-DM patients, but not in DM patients [74]. Hyperglycemia at admission was also associated with worse clinical outcomes in DM patients with poorly controlled blood sugar (hemoglobin A1c > 8.0%) [75]. In addition, metabolic syndrome was an important predictor of in-hospital mortality in STEMI patients, and the prognosis was worsen if DM or renal dysfunction was combined [76,77,78]. In metabolic syndrome patients with multi-vessel disease, coronary artery bypass graft had a favorable outcome in terms of revascularization compared with DES (4.8% vs. 12.2%, p = 0.014) [79]. However, there were no significant differences among different types of DES [53].
The estimated glomerular filtration rate (eGFR) was associated with both short- and long-term mortality rates in AMI patients [80,81], and the association between lower eGFR and mortality weakened with increasing age [82]. However, patients with renal dysfunction had a lower likelihood of receiving optimal medical care [83]. Early invasive strategies improved the prognosis in patients with renal dysfunction, with the exception of those with severe chronic kidney disease [84].
PCI for AMI yielded favorable outcomes, even in elderly patients [85,86,87]. Generally, the clinical status of octogenarians was significantly inferior to that of nonoctogenarians in terms of Killip class ≥ II (34.8% vs. 22.5%, p < 0.001), multivessel disease (65.8% vs. 53.7%, p < 0.001). The rate of 1-year all-cause death was significantly higher in octogenarians compared with nonoctogenarians (22.3% vs. 6.5%, p < 0.001) [88]. However, elderly (> 75 years) AMI patients with cardiogenic shock had a similar outcome after PCI as younger patients [89]. Nonagenarian AMI patients had similar outcomes as octogenarians, despite the higher in-hospital and 1-year mortality rates [87].
The KAMIR has generated a multitude of publications. In addition, the KAMIR score provides a simple and accurate assessment tool for improving risk stratification in contemporary clinical practice. The prognosis of AMI patients differs according to the presence of coronary risk factors, the time of arrival at the hospital, and clinical findings. Before the surgical procedure, a standard loading dose of clopidogrel was sufficient for most Korean patients. Low-molecular-weight heparin had a better clinical outcome than did unfractionated heparin. DES implantation in AMI patients reduced target lesion failure compared with BMS, and had similar safety profiles. Among DESs, everolimus-eluting and SESs showed better outcomes. Statins reduced adverse cardiac events, including stent thrombosis, irrespective of cholesterol levels. The addition of cilostazol to a dual antiplatelet agent improved clinical outcomes in patients with STEMI that experienced the no-reflow phenomenon during intervention. Individual patient factors, such as female gender, very old age, and chronic kidney disease, were associated with a poor clinical status, and such patients received guideline-directed treatments less frequently. However, thorough and appropriate management could improve the prognosis in these groups.
Acknowledgments
This study was performed with the support of the Korean Circulation Society (KCS) as a memorandum of the 50th Anniversary of the KCS. This study was supported by a grant of the Korean Health Technology R&D Project (HI13C1527), sponsored by the Ministry for Health and Welfare, Republic of Korea.
References
1. Kim HK, Jeong MH, Ahn Y, et al. A new risk score system for the assessment of clinical outcomes in patients with non-ST-segment elevation myocardial infarction. Int J Cardiol 2010;145:450–454PMID : 19541376.


2. Kim HK, Jeong MH, Ahn Y, et al. Hospital discharge risk score system for the assessment of clinical outcomes in patients with acute myocardial infarction (Korea Acute Myocardial Infarction Registry [KAMIR] score). Am J Cardiol 2011;107:965–971.e1PMID : 21256468.


3. Kim KH, Kim W, Hwang SH, et al. The CHADSVASc score can be used to stratify the prognosis of acute myocardial infarction patients irrespective of presence of atrial fibrillation. J Cardiol 2014;6. 24. [Epub]. http://dx.doi.org/10.1016/j.jjcc.2014.04.011.

4. Jeong YW, Jeong MH, Kim SS, et al. CHA2DS2-VASc scoring system as an initial method for screening high-risk patients in acute myocardial infarction. Int J Cardiol 2014;174:777–780PMID : 24767764.


5. Cho JY, Jeong MH, Ahn Y, et al. Impact of high admission blood pressure without history of hypertension on clinical outcomes of patients with acute myocardial infarction: from Korea Acute Myocardial Infarction Registry. Int J Cardiol 2014;172:e54–e58PMID : 24424340.


6. Kang DG, Jeong MH, Ahn Y, et al. Clinical effects of hypertension on the mortality of patients with acute myocardial infarction. J Korean Med Sci 2009;24:800–806PMID : 19794974.



7. Li YJ, Rha SW, Chen KY, et al. Clinical characteristics and mid-term outcomes of acute myocardial infarction patients with prior cerebrovascular disease in an Asian population: lessons from the Korea Acute Myocardial Infarction Registry. Clin Exp Pharmacol Physiol 2010;37:581–586PMID : 20105192.


8. Kim C, Chang HJ, Cho I, et al. Impact of family history on the presentation and clinical outcomes of coronary heart disease: data from the Korea Acute Myocardial Infarction Registry. Korean J Intern Med 2013;28:547–556PMID : 24009450.



9. Kang SH, Suh JW, Choi DJ, et al. Cigarette smoking is paradoxically associated with low mortality risk after acute myocardial infarction. Nicotine Tob Res 2013;15:1230–1238PMID : 23231825.


10. Chen KY, Rha SW, Li YJ, et al. 'Smoker's paradox' in young patients with acute myocardial infarction. Clin Exp Pharmacol Physiol 2012;39:630–635PMID : 22551379.


11. Kang WY, Jeong MH, Ahn YK, et al. Obesity paradox in Korean patients undergoing primary percutaneous coronary intervention in ST-segment elevation myocardial infarction. J Cardiol 2010;55:84–91PMID : 20122553.


12. Lee SH, Park JS, Kim W, et al. Impact of body mass index and waist-to-hip ratio on clinical outcomes in patients with ST-segment elevation acute myocardial infarction (from the Korean Acute Myocardial Infarction Registry). Am J Cardiol 2008;102:957–965PMID : 18929693.


13. Park HW, Yoon CH, Kang SH, et al. Early- and late-term clinical outcome and their predictors in patients with ST-segment elevation myocardial infarction and non-ST-segment elevation myocardial infarction. Int J Cardiol 2013;169:254–261PMID : 24071385.


14. Song YB, Hahn JY, Kim JH, et al. Comparison of angiographic and other findings and mortality in non-ST-segment elevation versus ST-segment elevation myocardial infarction in patients undergoing early invasive intervention. Am J Cardiol 2010;106:1397–1403PMID : 21059427.


15. Kim SS, Jeong MH, Rhew SH, et al. Impact of patients' arrival time on the care and in-hospital mortality in patients with non-ST-elevation myocardial infarction. Am J Cardiol 2014;113:262–269PMID : 24295548.


16. Park HE, Koo BK, Lee W, et al. Periodic variation and its effect on management and prognosis of Korean patients with acute myocardial infarction. Circ J 2010;74:970–976PMID : 20354338.


17. Song YB, Hahn JY, Gwon HC, et al. The impact of initial treatment delay using primary angioplasty on mortality among patients with acute myocardial infarction: from the Korea Acute Myocardial Infarction Registry. J Korean Med Sci 2008;23:357–364PMID : 18583867.



18. Lee JH, Chae SC, Yang DH, et al. Influence of weather on daily hospital admissions for acute myocardial infarction (from the Korea Acute Myocardial Infarction Registry). Int J Cardiol 2010;144:16–21PMID : 19403184.


19. Cho JY, Jeong MH, Ahn YK, et al. Comparison of outcomes of patients with painless versus painful ST-segment elevation myocardial infarction undergoing percutaneous coronary intervention. Am J Cardiol 2012;109:337–343PMID : 22088201.


20. Choi JS, Kim CS, Park JW, et al. Renal dysfunction as a risk factor for painless myocardial infarction: results from Korea Acute Myocardial Infarction Registry. Clin Res Cardiol 2012;101:795–803PMID : 22555520.


21. Kwon TG, Bae JH, Jeong MH, et al. N-terminal pro-B-type natriuretic peptide is associated with adverse short-term clinical outcomes in patients with acute ST-elevation myocardial infarction underwent primary percutaneous coronary intervention. Int J Cardiol 2009;133:173–178PMID : 18281115.


22. Kim CS, Kim MJ, Kang YU, et al. Influence of renal dysfunction on clinical outcomes in patients with congestive heart failure complicating acute myocardial infarction. Int Heart J 2013;54:304–310PMID : 24097221.


23. Kang YU, Kim MJ, Choi JS, et al. Concomitant impact of high-sensitivity C-reactive protein and renal dysfunction in patients with acute myocardial infarction. Yonsei Med J 2014;55:132–140PMID : 24339298.



24. Lee SH, Kim YJ, Kim W, et al. Clinical outcomes and therapeutic strategy in patients with acute myocardial infarction according to renal function: data from the Korean Acute Myocardial Infarction Registry. Circ J 2008;72:1410–1418PMID : 18724014.


25. Seo SM, Kim TH, Kim CJ, et al. Prognostic impact of significant non-infarct-related left main coronary artery disease in patients with acute myocardial infarction who receive a culprit-lesion percutaneous coronary intervention. Coron Artery Dis 2012;23:307–314PMID : 22527385.


26. Sim DS, Ahn Y, Jeong MH, et al. Clinical outcome of unprotected left main coronary artery disease in patients with acute myocardial infarction. Int Heart J 2013;54:185–191PMID : 23924928.


27. Kim U, Park JS, Kang SW, et al. Outcomes according to presentation with versus without cardiogenic shock in patients with left main coronary artery stenosis and acute myocardial infarction. Am J Cardiol 2012;110:36–39PMID : 22481010.


28. Baek JY, Seo SM, Park HJ, et al. Clinical outcomes and predictors of unprotected left main stem culprit lesions in patients with acute ST segment elevation myocardial infarction. Catheter Cardiovasc Interv 2014;83:E243–E250PMID : 22105969.


29. Kim MC, Ahn Y, Rhew SH, et al. Impact of total occlusion of an infarct-related artery on long-term mortality in acute non-ST-elevation myocardial infarction patients who underwent early percutaneous coronary intervention. Int Heart J 2012;53:160–164PMID : 22790683.


30. Kim SS, Choi HS, Jeong MH, et al. Clinical outcomes of acute myocardial infarction with occluded left circumflex artery. J Cardiol 2011;57:290–296PMID : 21388789.


31. Kang WY, Jeong MH, Ahn YK, et al. Are patients with angiographically near-normal coronary arteries who present as acute myocardial infarction actually safe? Int J Cardiol 2011;146:207–212PMID : 19664828.


32. Jeong HC, Ahn YK, Jeong MH, et al. Intensive pharmacologic treatment in patients with acute non ST-segment elevation myocardial infarction who did not undergo percutaneous coronary intervention. Circ J 2008;72:1403–1409PMID : 18724013.


33. Choo EH, Chang K, Ahn Y, et al. Benefit of beta-blocker treatment for patients with acute myocardial infarction and preserved systolic function after percutaneous coronary intervention. Heart 2014;100:492–499PMID : 24395980.


34. Jeong HC, Jeong MH, Ahn Y, et al. Comparative assessment of angiotensin II type 1 receptor blockers in the treatment of acute myocardial infarction: surmountable vs. insurmountable antagonist. Int J Cardiol 2014;170:291–297PMID : 24239100.


35. Jeong HC, Jeong JM, Jeong MH, et al. Effect of single or dual blockade of renin-angiotensin system in acute myocardial infarction patients according to renal function. Int J Cardiol 2012;157:408–411PMID : 22513185.



36. Kim JS, Kim CH, Chun KJ, et al. Effects of trimetazidine in patients with acute myocardial infarction: data from the Korean Acute Myocardial Infarction Registry. Clin Res Cardiol 2013;102:915–922PMID : 23982468.


37. Yang MJ, Lee HC, Lee HW, et al. Effect of nicorandil on clinical outcomes in patients with ST-segment elevation and non-ST-segment elevation myocardial infarction: based on the Korea Acute Myocardial Infarction Registry (KAMIR). Int J Cardiol 2013;168:4868–4869PMID : 23899744.


38. Kim JY, Jeong MH, Moon JH, et al. Impact of Clopidogrel loading dose in patients with chronic kidney disease undergoing primary percutaneous coronary intervention for ST-segment elevation myocardial infarction. Am J Cardiol 2012;110:1598–1606PMID : 22935526.


39. Choi CU, Rha SW, Oh DJ, et al. Standard versus high loading doses of clopidogrel in Asian ST-segment elevation myocardial infarction patients undergoing percutaneous coronary intervention: insights from the Korea Acute Myocardial Infarction Registry. Am Heart J 2011;161:373–382.e1-3PMID : 21315222.


40. Cho JS, Her SH, Baek JY, et al. Clinical benefit of low molecular weight heparin for ST-segment elevation myocardial infarction patients undergoing primary percutaneous coronary intervention with glycoprotein IIb/IIIa inhibitor. J Korean Med Sci 2010;25:1601–1608PMID : 21060749.



41. Li YJ, Rha SW, Chen KY, et al. Low-molecular-weight heparin versus unfractionated heparin in acute ST-segment elevation myocardial infarction patients undergoing primary percutaneous coronary intervention with drug-eluting stents. Am Heart J 2010;159:684–690.e1PMID : 20362730.


42. Li YJ, Rha SW, Chen KY, et al. Low molecular weight heparin versus unfractionated heparin in patients with acute non-ST-segment elevation myocardial infarction undergoing percutaneous coronary intervention with drug-eluting stents. J Cardiol 2012;59:22–29PMID : 22079855.


43. Sim DS, Jeong MH, Ahn Y, et al. Safety and benefit of early elective percutaneous coronary intervention after successful thrombolytic therapy for acute myocardial infarction. Am J Cardiol 2009;103:1333–1338PMID : 19427424.


44. Sim DS, Jeong MH, Ahn Y, et al. Benefit of percutaneous coronary intervention in early latecomers with acute ST-segment elevation myocardial infarction. Am J Cardiol 2012;110:1275–1281PMID : 22819423.


45. Kim MC, Jeong MH, Ahn Y, et al. What is optimal revascularization strategy in patients with multivessel coronary artery disease in non-ST-elevation myocardial infarction? Multivessel or culprit-only revascularization. Int J Cardiol 2011;153:148–153PMID : 20843572.


46. Lee HW, Hong TJ, Yang MJ, et al. Comparison of infarct-related artery vs multivessel revascularization in ST-segment elevation myocardial infarction with multivessel disease: analysis from Korea Acute Myocardial Infarction Registry. Cardiol J 2012;19:256–266PMID : 22641544.


47. Hong YJ, Jeong MH, Ahn Y, Kang JC. The efficacy and safety of drug-eluting stents in patients with acute myocardial infarction: results from Korea Acute Myocardial Infarction (KAMIR). Int J Cardiol 2013;163:1–4PMID : 22370372.


48. Sim DS, Jeong MH, Ahn Y, et al. Effectiveness of drug-eluting stents versus bare-metal stents in large coronary arteries in patients with acute myocardial infarction. J Korean Med Sci 2011;26:521–527PMID : 21468259.



49. Bae EH, Lim SY, Choi YH, et al. Drug-eluting vs. bare-metal stents for treatment of acute myocardial infarction with renal insufficiency: results from Korea Acute Myocardial Infarction Registry. Circ J 2011;75:2798–2804PMID : 22008317.


50. Lee SR, Jeong MH, Ahn YK, et al. Clinical safety of drug-eluting stents in the Korea acute myocardial infarction registry. Circ J 2008;72:392–398PMID : 18296834.


51. Cho Y, Yang HM, Park KW, et al. Paclitaxel- versus sirolimus-eluting stents for treatment of ST-segment elevation myocardial infarction: with analyses for diabetic and nondiabetic subpopulation. JACC Cardiovasc Interv 2010;3:498–506PMID : 20488406.


52. Kim HK, Jeong MH, Ahn YK, et al. Comparison of outcomes between Zotarolimus- and sirolimus-eluting stents in patients with ST-segment elevation acute myocardial infarction. Am J Cardiol 2010;105:813–818PMID : 20211324.


53. Lee MG, Jeong MH, Ahn Y, et al. Comparison of paclitaxel-, sirolimus-, and zotarolimus-eluting stents in patients with acute ST-segment elevation myocardial infarction and metabolic syndrome. Circ J 2011;75:2120–2127PMID : 21757819.


54. Chen KY, Rha SW, Wang L, et al. Unrestricted use of 2 new-generation drug-eluting stents in patients with acute myocardial infarction: a propensity score-matched analysis. JACC Cardiovasc Interv 2012;5:936–945PMID : 22995881.


55. Cho SC, Jeong MH, Kim W, et al. Clinical outcomes of everolimus- and zotarolimus-eluting stents in patients with acute myocardial infarction for small coronary artery disease. J Cardiol 2014;63:409–417PMID : 24314902.


56. Ahmed K, Jeong MH, Chakraborty R, et al. Role of intravascular ultrasound in patients with acute myocardial infarction undergoing percutaneous coronary intervention. Am J Cardiol 2011;108:8–14PMID : 21529735.


57. Hachinohe D, Jeong MH, Saito S, et al. Clinical impact of thrombus aspiration during primary percutaneous coronary intervention: results from Korea Acute Myocardial Infarction Registry. J Cardiol 2012;59:249–257PMID : 22341434.


58. Lee JH, Yang DH, Park HS, et al. Suboptimal use of evidence-based medical therapy in patients with acute myocardial infarction from the Korea Acute Myocardial Infarction Registry: prescription rate, predictors, and prognostic value. Am Heart J 2010;159:1012–1019PMID : 20569714.


59. Lee JH, Park HS, Chae SC, et al. Predictors of six-month major adverse cardiac events in 30-day survivors after acute myocardial infarction (from the Korea Acute Myocardial Infarction Registry). Am J Cardiol 2009;104:182–189PMID : 19576343.


60. Lee CH, Lee SH, Park JS, et al. Impact of statin usage patterns on outcomes after percutaneous coronary intervention in acute myocardial infarction: Korea Working Group on Myocardial Infarction registry (KorMI) study. J Geriatr Cardiol 2014;11:93–99PMID : 25009557.



61. Cho KH, Jeong MH, Ahn Y, et al. Low-density lipoprotein cholesterol level in patients with acute myocardial infarction having percutaneous coronary intervention (the cholesterol paradox). Am J Cardiol 2010;106:1061–1068PMID : 20920639.


62. Lee KH, Jeong MH, Kim HM, et al. Benefit of early statin therapy in patients with acute myocardial infarction who have extremely low low-density lipoprotein cholesterol. J Am Coll Cardiol 2011;58:1664–1671PMID : 21982310.


63. Jeong HC, Ahn Y, Hong YJ, et al. Statin therapy to reduce stent thrombosis in acute myocardial infarction patients with elevated high-sensitivity C-reactive protein. Int J Cardiol 2013;167:1848–1853PMID : 22592028.


64. Lim SY, Bae EH, Choi JS, et al. Effect on short- and long-term major adverse cardiac events of statin treatment in patients with acute myocardial infarction and renal dysfunction. Am J Cardiol 2012;109:1425–1430PMID : 22356794.


65. Chen KY, Rha SW, Li YJ, et al. Triple versus dual antiplatelet therapy in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Circulation 2009;119:3207–3214PMID : 19528339.


66. Choo EH, Kim PJ, Chang K, et al. The impact of no-reflow phenomena after primary percutaneous coronary intervention: a time-dependent analysis of mortality. Coron Artery Dis 2014;25:392–398PMID : 24625688.


67. Lee KH, Ahn Y, Kim SS, et al. Comparison of triple anti-platelet therapy and dual anti-platelet therapy in patients with acute myocardial infarction who had no-reflow phenomenon during percutaneous coronary intervention. Circ J 2013;77:2973–2981PMID : 23986083.


68. Korea Acute Myocardial Infarction Registry (KAMIR) Investigators. Lee KH, Jeong MH, et al. Gender differences of success rate of percutaneous coronary intervention and short term cardiac events in Korea Acute Myocardial Infarction Registry. Int J Cardiol 2008;130:227–234PMID : 18077018.


69. Park JS, Kim YJ, Shin DG, et al. Gender differences in clinical features and in-hospital outcomes in ST-segment elevation acute myocardial infarction: from the Korean Acute Myocardial Infarction Registry (KAMIR) study. Clin Cardiol 2010;33:E1–E6PMID : 20589943.



70. Woo JS, Kim W, Ha SJ, Kim SJ, Kang WY, Jeong MH. Impact of gender differences on long-term outcomes after successful percutaneous coronary intervention in patients with acute myocardial infarction. Int J Cardiol 2010;145:516–518PMID : 20394997.


71. Kang SH, Suh JW, Yoon CH, et al. Sex differences in management and mortality of patients with ST-elevation myocardial infarction (from the Korean Acute Myocardial Infarction National Registry). Am J Cardiol 2012;109:787–793PMID : 22196789.


72. Kim HL, Kang SH, Yoon CH, et al. Differential prognostic impacts of diabetes over time course after acute myocardial infarction. J Korean Med Sci 2013;28:1749–1755PMID : 24339704.



73. Park KH, Ahn Y, Jeong MH, et al. Different impact of diabetes mellitus on in-hospital and 1-year mortality in patients with acute myocardial infarction who underwent successful percutaneous coronary intervention: results from the Korean Acute Myocardial Infarction Registry. Korean J Intern Med 2012;27:180–188PMID : 22707890.



74. Yang JH, Song PS, Song YB, et al. Prognostic value of admission blood glucose level in patients with and without diabetes mellitus who sustain ST segment elevation myocardial infarction complicated by cardiogenic shock. Crit Care 2013;17:R218. PMID : 24090250.



75. Lee SA, Cho SJ, Jeong MH, et al. Hypoglycemia at admission in patients with acute myocardial infarction predicts a higher 30-day mortality in patients with poorly controlled type 2 diabetes than in well-controlled patients. Diabetes Care 2014;37:2366–2373PMID : 24914243.


76. Lee MG, Jeong MH, Ahn Y, et al. Impact of the metabolic syndrome on the clinical outcome of patients with acute ST-elevation myocardial infarction. J Korean Med Sci 2010;25:1456–1461PMID : 20890426.



77. Lee MG, Jeong MH, Ahn Y, et al. Additive impact of diabetes mellitus on patients with metabolic syndrome and acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Int J Cardiol 2012;157:283–285PMID : 22483421.


78. Kim CS, Choi JS, Bae EH, et al. Association of metabolic syndrome and renal insufficiency with clinical outcome in acute myocardial infarction. Metabolism 2013;62:669–676PMID : 23218489.


79. Ahmed K, Jeong MH, Chakraborty R, et al. Percutaneous coronary intervention with drug-eluting stent implantation vs. coronary artery bypass grafting for multivessel coronary artery disease in metabolic syndrome patients with acute myocardial infarction. Circ J 2012;76:721–728PMID : 22240598.


80. Bae EH, Lim SY, Cho KH, et al. GFR and cardiovascular outcomes after acute myocardial infarction: results from the Korea Acute Myocardial Infarction Registry. Am J Kidney Dis 2012;59:795–802PMID : 22445708.


81. Choi JS, Kim CS, Bae EH, et al. Predicting outcomes after myocardial infarction by using the Chronic Kidney Disease Epidemiology Collaboration equation in comparison with the Modification of Diet in Renal Disease study equation: results from the Korea Acute Myocardial Infarction Registry. Nephrol Dial Transplant 2012;27:3868–3874PMID : 22879394.


82. Choi JS, Kim MJ, Kang YU, et al. Association of age and CKD with prognosis of myocardial infarction. Clin J Am Soc Nephrol 2013;8:939–944PMID : 23430208.



83. Choi JS, Kim CS, Bae EH, et al. Suboptimal medical care of patients with ST-elevation myocardial infarction and renal insufficiency: results from the Korea Acute Myocardial Infarction Registry. BMC Nephrol 2012;13:110. PMID : 22966970.




84. Hachinohe D, Jeong MH, Saito S, et al. Management of non-ST-segment elevation acute myocardial infarction in patients with chronic kidney disease (from the Korea Acute Myocardial Infarction Registry). Am J Cardiol 2011;108:206–213PMID : 21712106.


85. Lim SY, Bae EH, Choi JS, et al. Percutaneous coronary intervention for acute myocardial infarction in elderly patients with renal dysfunction: results from the Korea Acute Myocardial Infarction Registry. J Korean Med Sci 2013;28:1027–1033PMID : 23853485.



86. Piao ZH, Jeong MH, Jin L, et al. Clinical impact of early intervention in octogenarians with non-ST-elevation myocardial infarction. Int J Cardiol 2014;172:462–464PMID : 24512878.


87. Lee KH, Ahn Y, Kim SS, et al. Characteristics, in-hospital and long-term clinical outcomes of nonagenarian compared with octogenarian acute myocardial infarction patients. J Korean Med Sci 2014;29:527–535PMID : 24753700.



Figure 1
Korea Acute Myocardial Infarction Registry score for predicting 1-year mortality. PCI, percutaneous coronary intervention; LVEF, left ventricular ejection fraction.
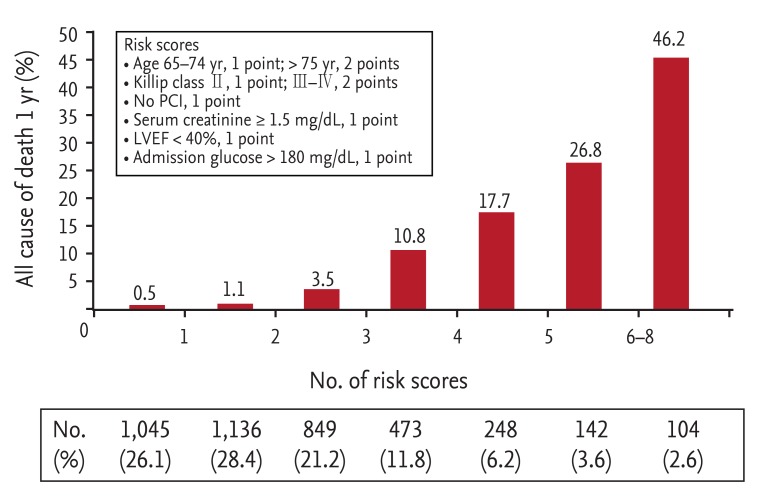
Figure 2
Major adverse cardiac events according to statin use in patients with very low low-density lipoprotein cholesterol levels. MACE, major adverse clinical events; PCI, percutaneous coronary intervention.
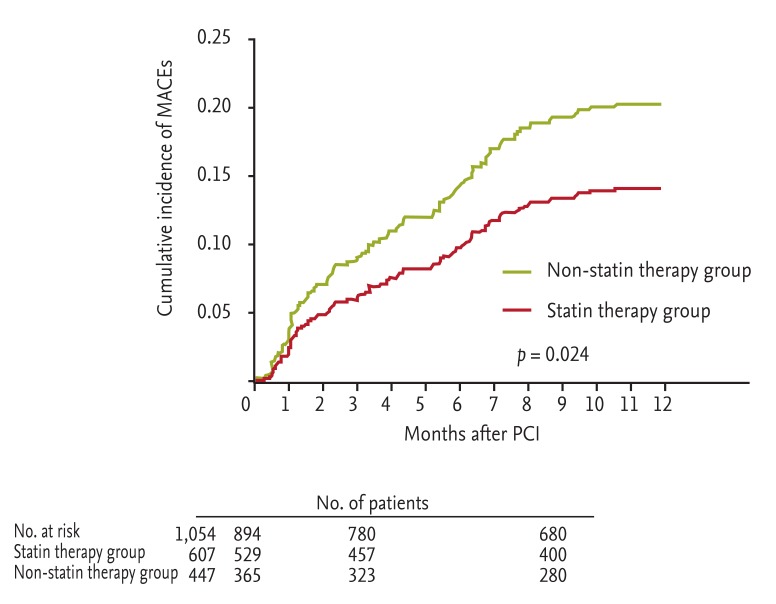
Table 2
Stent study summary in Korea Acute Myocardial Infarction Registry
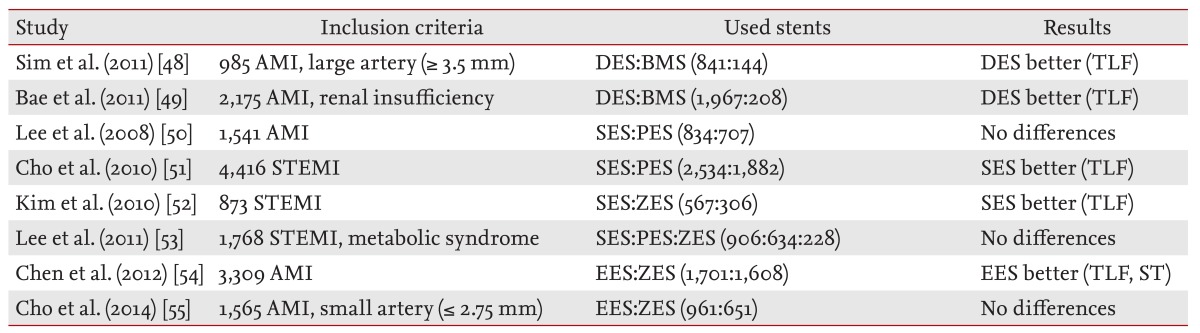
AMI, acute myocardial infarction; DES, drug-eluting stent; BMS, bare metal stent; TLF, target lesion failure; SES, sirolimus-eluting stent; PES, paclitaxel-eluting stent; STEMI, ST segment elevation myocardial infarction; ZES, zotarolimus-eluting stent; EES, everolimus-eluting stent; ST, stent thrombosis.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



