 |
 |
| Korean J Intern Med > Volume 28(3); 2013 > Article |
|
To the Editor,
Autoimmune diseases encompass a wide spectrum of disorders from organ specific to multisystemic involvement. Sometimes, autoimmune diseases coexist with each other and the overlap syndrome is defined by the development of clinical features of two or more autoimmune diseases simultaneously. There are a number of mechanisms implicated in the pathogenesis of these overlaps. Genetic factors, such as shared susceptible alleles, cross-reactivity of autoantibody, autoreactive T cell and cytokine imbalance have been suggested [1]. Hashimoto's thyroiditis is an organ specific autoimmune disorder. Its association with systemic autoimmune diseases has been described, including systemic lupus erythematosus, Sjögren syndrome, systemic sclerosis, and rheumatoid arthritis [2]. However, the occurrence of Hashimoto's thyroiditis and polymyositis is very rare and not well documented. We describe a 20-year-old woman with polymyositis who was diagnosed as Hashimoto's thyroiditis concomitantly.
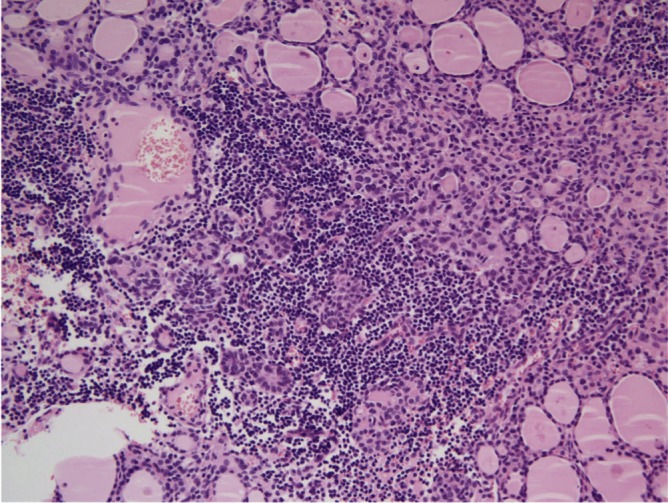
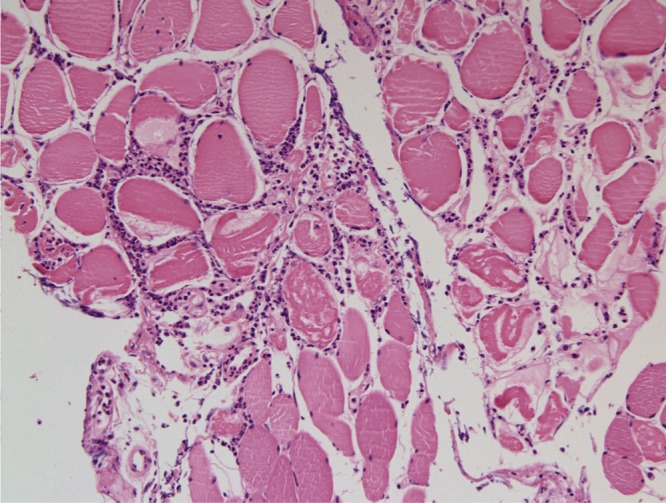
A 20-year-old woman was admitted to the hospital complaining of fever and pain with weakness in arms and thighs. Three months ago, she felt pain in the both extremities and had difficulty in standing, walking on stairs and rising arms over the head. At admission, blood pressure was 100/60 mmHg, heart rate was 110 beats per minute, and temperature was 39℃. Thyroid gland was diffusely enlarged with a smooth surface and soft consistency. Musculoskeletal examination revealed tenderness in all four extremities. Muscle strength of the extremities was 3 to 4/5 in arms and 3/5 in legs. On neurological examination, sensation, and deep tendon reflexes were normal or intact. Laboratory findings were as follows: white blood cell 23,180/mm3, hemoglobin 9.1 g/dL, platelet 511,000/mm3, erythrocyte sedimentation rate 58 mm/hr, C-reactive protein 10.4 mg/dL, serum total protein 8.5 g/dL, albumin 4.4 g/dL, aspartate transaminase (AST) 55 IU/L, creatinine 0.82 mg/dL, lactate dehydrogenase 1,296 IU/L (normal range, 218 to 472), creatine phosphokinase (CPK) 386 IU/L (normal range, 30 to 334), and aldolase 7.6 U/mL (normal range, 2 to 8). Thyroid stimulating hormone was 2.39 µU/mL (normal range, 0.35 to 5.50), free T4 1.03 ng/dL (normal range, 0.89 to 1.80), antithyroglobulin 732 IU/mL (normal range, 0 to 40), antimicrosomal antibody 245 IU/mL (normal range, 0 to 25), and thyroid stimulating immunoglobulin was 5% (normal range, 0 to 15). Immunological examination revealed the following: antinuclear antibody positive at 1 : 40 in speckled pattern, rheumatoid factor, anti-SSA, anti-SSB, anti-dsDNA antibody, anti-Scl-70 antibody, antiribonuclear protein and anti-Jo-1 antibody were all negative. Ultrasonogram of the thyroid gland demonstrated diffuse enlargement of the thyroid gland and 1 cm sized hypovascular echogenic nodule on right upper pole. An electromyography (EMG) finding was occasional small fasciculations and polyphasic motor unit potentials of low amplitude and short duration, suggestive of myopathy. Histological examination of the resected thyroid right lobe revealed follicular cell proliferative lesions in background of parenchymal extensive mononuclear inflammatory cell infiltration and oxyphilic changes of follicular epithelium, consistent with nodular hyperplasia in Hashimoto's thyroiditis (Fig. 1). Muscle biopsy specimen from the quadriceps showed necrotic and regenerating various sized muscle fiber and phagocytosis with endomyseal inflammatory cell infiltration and the perivascular infiltration of mononuclear cells, consistent with polymyositis (Fig. 2). She was diagnosed as having polymyositis and Hashimoto's thyroiditis and was treated with prednisolone (50 mg/day) and methotrexate (10 mg/wk). Her symptoms remarkably improved after treatment. Fever and myalgia disappeared quickly and muscle strength improved gradually.
This case showed some difficulties of interpreting laboratory data. Although, the levels of certain muscle enzyme (AST and CPK) were not so high at initial evaluation. The diagnosis of polymyositis was made by clinical, histological, and EMG findings. The conceivable explanation of these laboratory ambiguities lies in the use of corticosteroid for several weeks before the test.
Although the pathogenesis and the nature of the relationship between thyroid autoimmunity and autoimmune diseases is not completely established, some hypotheses may be implicated: 1) immune modulatory effects of antithyroid antibodies; 2) molecular mimicry between thyroid and disease specific epitopes; and 3) genetic link between antithyroid autoimmunity and the susceptibility to autoimmune disease [2]. Cross-reactivity of antithyroid antibodies or autoreactive T cells with other organs and cytokine imbalance may also implicated [2,3]. About 2% of inflammatory myopathy patients exerted thyroid autoimmunity. Suppressor T cell dysfunction and lymphocyte mediated cytotoxicity have been described in patient with polymyositis and there are some evidences of suppressor T cell dysfunction in autoimmune thyroiditis [2,4]. It could be hypothesized that coexisting autoimmune thyroiditis and inflammatory myopathy develop from the common autoimmune pathogenic mechanism.
In conclusion, systemic and thyroid autoimmune diseases may overlap with each other. It is important to be aware that polymyositis and autoimmune thyroiditis can coexist and a thorough evaluation of both conditions may be necessary in patients presenting with myalgia or muscle weakness.
References
1. Shoenfeld Y, Isenberg DA. The mosaic of autoimmunity. Immunol Today 1989;10:123–126PMID : 2665774.


2. Biro E, Szekanecz Z, Czirjak L, et al. Association of systemic and thyroid autoimmune diseases. Clin Rheumatol 2006;25:240–245PMID : 16247581.


-
METRICS

-
- 1 Crossref
- 0 Scopus
- 9,354 View
- 64 Download
- Related articles
-
Abnormal ectodermal findings associated with gastrointestinal polyposis2016 September;31(5)
Gastric polyposis associated with portal hypertension2013 March;28(2)
A Case of Polychondritis in a Patient with Behçet's Disease2005 December;20(4)



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print


