INTRODUCTION
Riedel's thyroiditis (RT) is a rare form of thyroiditis that may be related to a diverse range of clinical symptoms. It has been reported in approximately 0.06% of patients who undergo surgery for an abnormality in the thyroid gland [1]. Although it has been assumed to be one of the clinical manifestations of multifocal fibrosclerosis, its cause has not been clearly determined. As it can easily be confused with a malignant tumor, diagnosis prior to surgical excision of the thyroid gland is difficult. For definitive diagnosis, histopathologic analysis of the thyroid gland is necessary [2]. Reports of this disorder in Korea are extremely rare and only a few cases with concurrent presence of RT and other thyroid diseases have so far been reported [2-4]. There have been no reports of RT accompanied by acute suppurative thyroiditis and micropapillary carcinoma.
We report, together with a review of the literature, a single case of RT accompanied by an abscess and micropapillary carcinoma diagnosed by surgical biopsy in a 48-year-old female patient who visited our hospital complaining of a neck mass with pain accompanied by cervical lymphadenopathy. Surgical biopsy was carried out because of difficulties in ruling out a malignant tumor due to the clinical characteristics.
CASE REPORT
A 48-year-old woman visited our hospital due to abdominal pain and fever of 3 days' duration. She received antibiotic treatment under the diagnosis of cholecystitis with gallstones and liver cirrhosis. The patient began to experience pain and swelling in the anterior neck region at the time of hospitalization. As her symptoms became aggravated, she was referred to the endocrinology department. The patient's history revealed the consumption of a bottle of alcohol five times a week over the previous 20 years. The remainder of her medical history was unremarkable.
At the time of consultation, the patient's blood pressure was 130/60 mmHg, her heart rate was 68 beats/min, and her body temperature was 37.6Ōäā. She was alert but had an acute ill-looking appearance. Jaundice was observed in the sclera and a 3 ├Ś 3 cm hard mass fixed around the right anterior area of the neck, accompanied by tenderness and enlargement of adjacent cervical lymph nodes, was palpated. The patient complained of abdominal pain and had direct tenderness in the right upper quadrant of her abdomen. There was no palpable organ or mass in the abdomen.
Laboratory examinations showed a hemoglobin count of 10.7 g/dL, a leukocyte count of 11,100/mm3 (neutrophils 76.0%, lymphocytes 17.0%, monocytes 3.4%, and eosinophils 1.1%), a thrombocyte count of 101,000/mm3, an aspartate aminotransferase level of 84 IU/L, an alkaline aminotransferase level of 40 IU/L, an alkaline phosphatase level of 311 IU/L, a total protein and albumin level of 6.7/2.3 g/dL, a total bilirubin level of 6.5 mg/dL, a glucose level of 114 mg/dL, a ╬│-GT level of 141 IU/L, a prothrombin time of 20.9 seconds (46%), an erythrocyte sedimentation rate of 120 mm/hr, and a C-reactive protein level of 4.42 mg/dL. Moreover, the serum thyroid stimulating hormone level was 1.23 mIU/L (normal range, 0.17 to 4.05), the T3 level 36.0 ng/dL (normal range, 60.0 to 190.0), the free T4 level 1.09 ng/dL (normal range, 0.80 to 1.90), the thyroglobulin antibody (Ab) level 113.71 U/mL (normal range, 0.00 to 100.00), and the microsomal Ab level 4.0 U/mL (normal range, 0.0 to 70.0). Blood culture carried out at the time of hospitalization showed growth of Escherichia coli and urine culture showed growth of Enterococcus species, which led to treatment with piperacillin/tazobactam and amikacin.
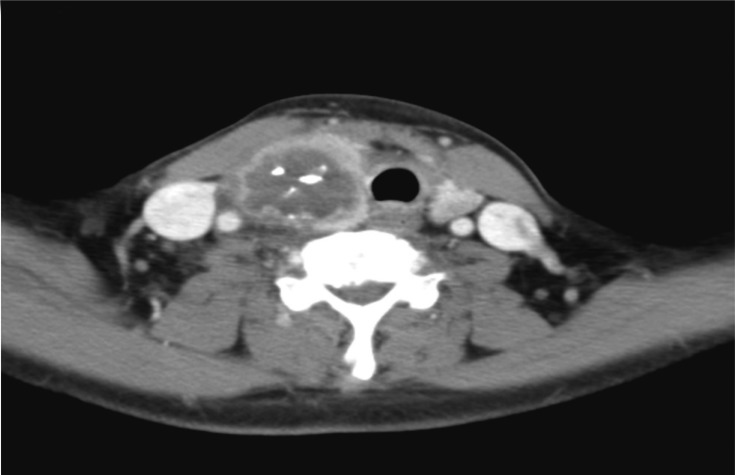
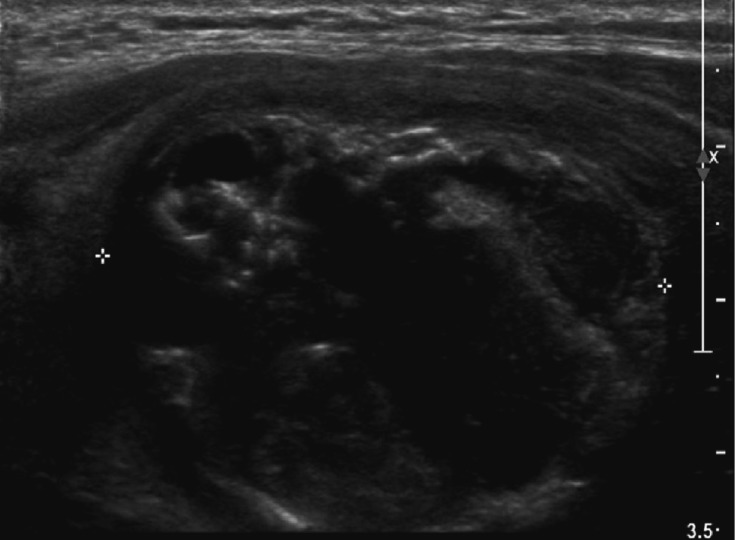
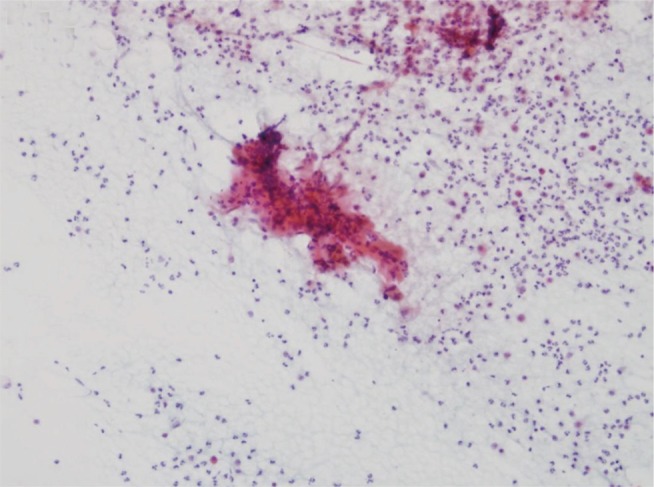
The chest X-ray was normal. Cervical computed tomography revealed a large nodular lesion of the right thyroid lobe with internal calcification and an irregular border, suggesting a malignant nodule. There was swelling and liquid collection in the surrounding soft tissue, which seemed to be due to accompanying hemorrhage or inflammation. Cervical lymphadenopathy of the level II lymph nodes on both sides and the level III and IV lymph nodes on the right side was observed (Fig. 1). Positron emission tomography revealed strong fluorodeoxyglucose (FDG) uptake by a large nodule of the right thyroid lobe and cervical lymphadenopathy at the left level IB lymph nodes, the level II lymph nodes on both sides, and the right level III, IV, and V areas, with strong FDG uptake. The results suggested malignancy of the right thyroid gland and abnormal cervical lymphadenopathy. On the basis of these findings, neck ultrasonography and ultrasound-guided fine needle aspiration biopsy (FNAB) were carried out. A 3.06 ├Ś 2.63 ├Ś 3.91 cm heterogeneous hypoechoic mass with calcification was observed in the right lobe of the thyroid gland, and FNAB was performed (Fig. 2). Aspiration of the nodule collected 10 mL of puslike fluid. Aspiration cytology results revealed no thyroid follicles, but fibrous tissues and spindle cells with numerous neutrophils, lymphocytes, and macrophages were observed (Fig. 3). Culture of the aspirated fluid resulted in the growth of E. coli.
After antibiotic therapy for acute suppurative thyroiditis, follow-up ultrasound-guided FNAB for the thyroid nodule was carried at 2 months. Ultrasonographic findings revealed a 3.4 ├Ś 3.6 ├Ś 3.5 cm hypoechoic nodule accompanied by calcification in the right thyroid lobe, suggesting a malignant nodule. Metastasis to the cervical lymph nodes was also suspected since the level II lymph nodes of the right cervical region were enlarged to 1.2 cm and hyperechoic findings suggested internal calcification. Cytologic analysis of the right thyroid nodule showed no evidence of malignancy. No follicle cells were seen; only a mixture of various inflammatory cells was observed. Ultrasound-guided FNAB was repeated a total of five times as the possibility of malignancy could not be ruled out. There was a single report of suspicion of malignancy and the other four biopsies resulted in a benign diagnosis or insufficient specimens. Surgical biopsy was recommended since anaplastic carcinoma accompanied by inflammation could not be ruled out. Surgical biopsy was performed for accurate histological diagnosis and treatment.
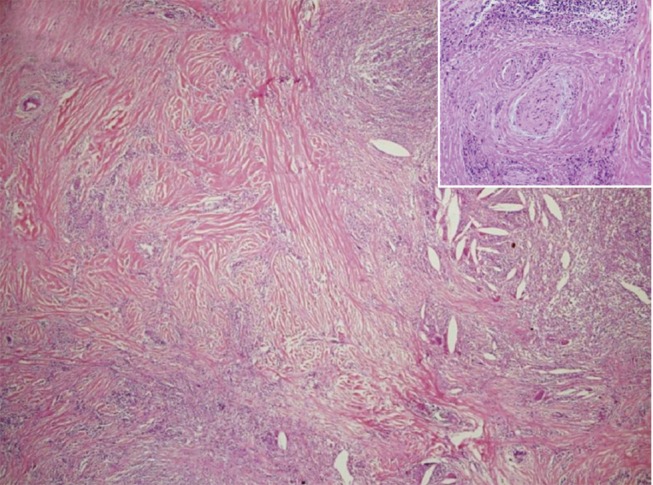
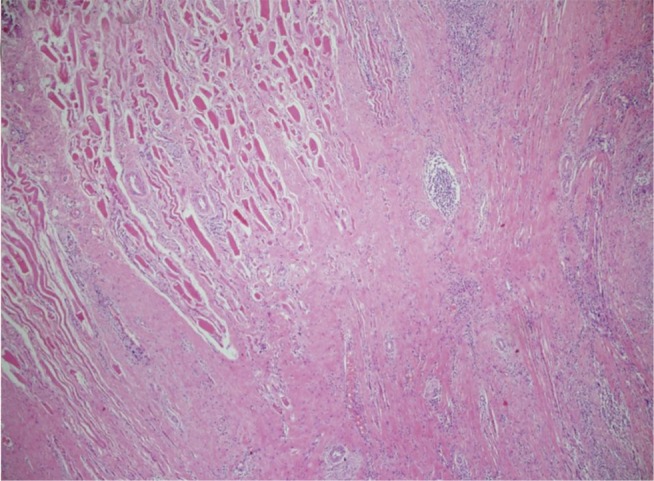
Analysis of a frozen biopsy section revealed a benign inflammatory disorder. However, since the possibility of malignancy could not be ruled out, total thyroidectomy and excision of the central cervical lymph nodes was performed. During the operation, a large hard nodule with adhesion to neighboring structures, including adjacent muscles and the internal jugular vein, was found in the right thyroid lobe. On gross examination, the cut surface revealed a hard grayish brown nodule with fibrosis, accompanied by multifocal necrosis and calcification. Histologic examination revealed loss or contraction of normal thyroid follicles of the right thyroid gland due to severe fibrosis, and many areas affected by localized abscesses, cholesterol crystallization, degenerative calcification, and infiltration of acute and chronic inflammatory cells (Fig. 4). In addition, the characteristic findings of chronic inflammation and fibrous tissues encasing a medium-sized vein were observed (Fig. 4, inset). Fibrous tissues and inflammation infiltrated the skeletal muscles around the thyroid gland (Fig. 5). In the left thyroid gland, a 0.15 cm micropapillary carcinoma was observed. On the basis of these findings, RT accompanied by acute suppurative thyroiditis and micropapillary carcinoma was diagnosed. The patient is currently being treated on an outpatient basis with thyroid hormone replacement therapy (150 ┬Ąg of levothyroxine per day).
DISCUSSION
RT is an extremely rare chronic inflammatory disorder of the thyroid gland, the cause of which is yet to be definitively defined. Its prevalence is three times higher in females than in males. The average age at the time of diagnosis is 50 years [1]. This disorder is mainly characterized by sudden enlargement of the thyroid gland (goiter) with palpation of a substantially hard mass and replacement of the normal thyroid gland parenchyma with very dense fibrous tissues. Although distinguishing RT from thyroid carcinoma is important in diagnostic evaluation, it is not possible to make the diagnosis with only clinical findings. Therefore, one relies on histological diagnosis at initial diagnosis since RT can be easily confused with malignant tumors, including thyroidal papillary carcinoma, lymphoma, and undifferentiated thyroid cancer, because of its clinical characteristics. In the majority of cases, it is not easy to obtain appropriate tissue samples by FNAB. FNAB itself is very difficult because the tissues are very hard and, even if some of the fibrotic tissue can be biopsied, there is a possibility that hidden malignant tumor cells would remain without being biopsied. Therefore, surgical biopsy is carried out together with treatment [2], as was done in this case.
The majority of surgical findings indicate that complete removal is very difficult because the stony hard fibrosis usually infiltrates the thyroid gland, respiratory tract, cervical muscles, esophagus, and nerve plexus. Therefore, the risk of damage to the parathyroid and recurrent laryngeal nerve is very high. In addition, an underlying malignant tumor or simultaneous thyroid adenoma may remain, as complete excision may be impossible due to fibrosis and invasion, necessitating continuous follow-up observation after surgery [3]. The present case involved invasion of neighboring structures, including muscles and the internal jugular vein, and surgery resulted in damage to the right parathyroid gland and right recurrent laryngeal nerve.
Microscopic findings in RT are characterized by the spread of fibrosis beyond the thyroid capsule and maintenance of relatively normal tissues in the noninvolved region. There may be occlusive phlebitis resulting from diffuse infiltration of the veins by lymphoid or fibrous tissue. Diagnoses that need to be pathologically distinguished include the fibrosing variant of Hashimoto's thyroiditis and paucicellular variant of anaplastic carcinoma. With the fibrosing variant of Hashimoto's thyroiditis, the fibrosis does not extend beyond the thyroid and does not cause phlebitis. It is also uncommon for the normal thyroid follicles to be preserved due to lymphocytic inflammation of the majority of the thyroid gland [5]. The paucicellular variant of anaplastic carcinoma is distinguished from RT as it presents with nontypical spindle cells, occlusion of large vessels by tumor cells, and immune reaction against epithelial markers [6]. Immunohistochemical staining is also helpful in differential diagnosis. Solitary fibrous tumor is distinguished by positive findings in its reaction against CD34 and Bcl-2. The paucicellular variant of anaplastic carcinoma is distinguished by the presence of a dense fibrous stroma that displays positive findings in cytokeratin (Ck) immunostaining against AE1, AE3, CAM5.2, Ck7, pan-Ck (Ck5, Ck6, Ck8, and Ck17), and Ck19 [7].
In the present case, RT was additionally accompanied by acute suppurative thyroiditis. Acute thyroiditis is rare because the thyroid gland has a capsule and an abundant blood supply, lymph nodes, and iodine, which has antibacterial actions. Although the infection route cannot be definitively defined in many cases, the major routes include direct propagation as the result of spread of infection from the surrounding cervical tissues and distant propagation through the lymphatics or the blood stream. Although ultrasonography, computed tomography, and magnetic resonance imaging can be helpful in diagnosis, a definitive diagnosis is achieved by Gram staining and culture of pus from the abscess [8]. Treatment includes administration of antibiotics appropriate for the cultured bacteria. If there is no clinical improvement, excision or drainage of the abscess is necessary.
Staphylococcus aureus is the most common pathogen causing the disorder, with group A ╬▓-hemolytic streptococcus the most common pathogen in the case of infants. Moreover, the disorder can also be caused by infection with E. coli and Pseudomonas aeruginosa; chronic infection by Treponema pallidum, tubercle bacillus, actinomycosis and Salmonella typhi; and parasitic infection by Echinococcus spp. and fungal infection by Aspergillus spp. [9]. In the present case, E. coli was identified from the aspirate from the abscess. Reports of suppurative thyroiditis due to E. coli are rare. In 1977, Saksouk and Salti [10] described acute suppurative thyroiditis caused by E. coli in a patient with a urinary tract infection as the main source of infection. In our case, since there was cholecystitis accompanied by gall stones and E. coli in the blood culture, it was likely the infection was propagated through the blood stream. Excision or drainage of the abscess was not performed due to clinical improvement after antibiotic use.
RT has recently been recognized as one of the manifestations of multifocal fibrosclerosis, which is characterized by fibrosis involving multiple organ systems, such as retroperitoneal fibrosis, mediastinal fibrosis, orbital tumors, pulmonary fibrosis, sclerosing cholangitis, and fibrous mumps [4]. In the present case, fibrosclerosis was not observed in other areas.
In summary, a patient visited our hospital with a tender cervical mass accompanied by cervical lymphadenopathy. Since the radiologic findings were suggestive of a thyroid malignancy, she was initially suspected to have a malignant tumor and acute suppurative thyroiditis. However, repeated FNAB did not reveal definitive findings that allowed us to diagnose a malignancy, and the patient was instead diagnosed with RT accompanied by abscesses and micropapillary carcinoma after surgical biopsy. A prudent diagnostic approach is needed for RT since differential diagnosis with other malignant tumors is clinically difficult. There is also a need for close and continuous follow-up of patients since surgical excision may be incomplete, and because of the possibility of a dormant cancer or of RT being a manifestation of multifocal fibrosclerosis, with other manifestations becoming evident later on.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print





