 |
 |
| Korean J Intern Med > Volume 27(3); 2012 > Article |
|
To the Editor,
Bowel endometriosis is defined as the presence of endometrial glands and stroma infiltrating the bowel wall reaching at least the subserous fat or adjacent to the neurovascular branches (subserous plexus) [1]. In general, colonoscopy offers little assistance in the diagnosis of bowel endometriosis because the lesions are typically submucosal and usually not visible during this examination [2].
A 48-year-old woman was referred to our hospital for further evaluation of an incidental submucosal tumor detected during colonoscopy for a health checkup. Recently, she had been suffering from cyclic, intractable pelvic pain, which was not associated with altered bowel habit or rectal bleeding. The physical examination revealed no specific findings, such as abdominal tenderness or palpable masses in the abdomen.
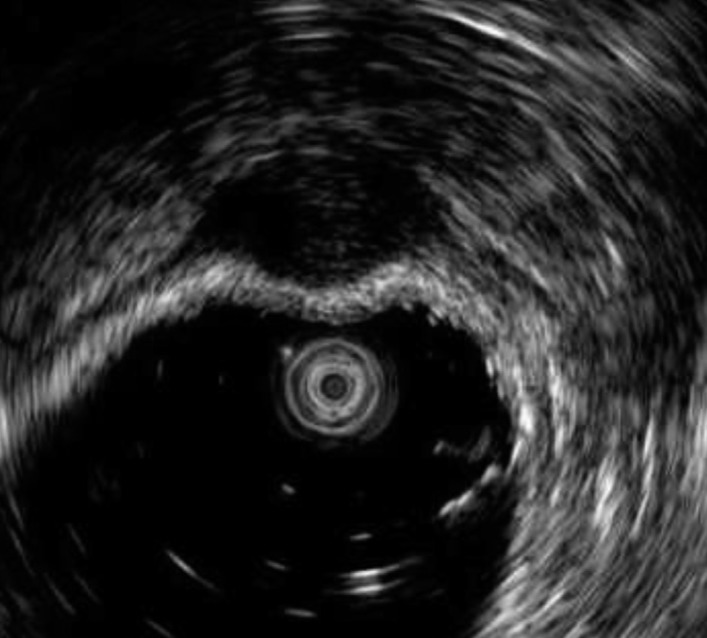
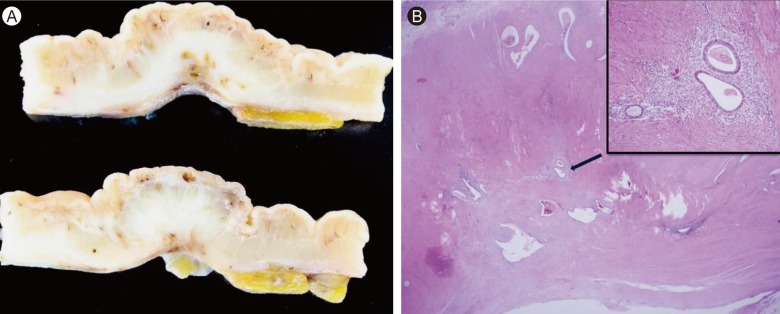
The laboratory examination showed an elevated cancer antigen (CA) 125 level at 110 IU/mL, while other values were within the normal limits. The gynecologic examination revealed a normal vagina, uterus, and uterine cervix. Transvaginal ultrasonography revealed multiple myomas in the uterine wall, but no abnormalities in either ovary. Abdominopelvic computed tomography showed no specific findings. Colonoscopy showed subepithelial compression with a smooth mucosal surface in the sigmoid colon 25 cm from the anal verge (Fig. 1). An endoscopic ultrasonography (EUS) miniprobe (UM-2R, Olympus Japan, Tokyo, Japan) was used to evaluate the subepithelial mass at a frequency of 12 MHz. This demonstrated a homogenous, hypoechoic, indistinctly shaped lesion located in the fourth layer (muscularis propria) (Fig. 2). Based on the EUS miniprobe findings, the possibility of a myogenic tumor, such as a leiomyoma or gastrointestinal stromal tumor, was considered in the differential diagnosis, but the presence of bowel endometriosis, although though to be less probable, could not be excluded with certainty. Bowel endometriosis had to be ruled out because the patient had cyclic, intractable pelvic pain; the CA-125 level was elevated at 110 IU/mL; and the location was the sigmoid colon. The patient underwent laparoscopy-assisted sigmoidectomy to confirm the diagnosis. Normal-appearing peritoneum was found at laparoscopy. The gross examination of the resected sigmoid colon revealed a 1.3-cm ill-defined hard mass in the wall, indenting the overlying serosal surface (Fig. 3A). No remarkable findings were noted in the mucosal surface. The mass consisted of an irregularly thickened proper muscle layer. Histologically, the mass consisted of irregularly arranged, proliferated smooth muscle cells of the proper muscle layer with embedded endometrial glands and stromal cells, consistent with bowel endometriosis (Fig. 3B).
On EUS, bowel endometriosis consists of heterogeneous or hypoechoic crescent-shaped lesions, involving the serosal, muscularis propria, and occasionally submucosal layers and sparing the mucosal layers [3-5]. Bowel endometriosis shows thickening of the muscularis propria and fibrotic adhesions and convergence of the serosa. This appears to be responsible for the typical EUS pattern. The heterogeneous echo finding is caused by the presence of the so-called chocolate cysts that result from hemorrhage within the implants induced by the hormonal cycle [4]. Bowel endometriosis often extends outside the rectal wall into the rectovaginal septum or into the posterior lower uterine wall; this infiltrative quality of the implants can be mistaken for a malignant process [4]. EUS is even less accurate for endometriotic nodules located away from the EUS probe, such as endometriosis in the uterosacral ligaments and ovaries. The accuracy for detection of nodules in the uterosacral ligaments or ovaries is 56% and 53%, respectively [3]. In our case, the normal-appearing peritoneum on laparoscopy was thought to explain the isolated bowel endometriosis, rather than missing perirectosigmoid endometriosis. In summary, this case report demonstrates that bowel endometriosis should be added to the shortlist of diseases that cause hypoechoic lesions located on the muscularis layer on EUS examination, of which the characteristic lesion is a myogenic tumor.
References
1. Remorgida V, Ferrero S, Fulcheri E, Ragni N, Martin DC. Bowel endometriosis: presentation, diagnosis, and treatment. Obstet Gynecol Surv 2007;62:461ŌĆō470PMID : 17572918.


2. Redwine DB, Sharpe DR. Laparoscopic surgery for intestinal and urinary endometriosis. Baillieres Clin Obstet Gynaecol 1995;9:775ŌĆō794PMID : 8821255.


3. Delpy R, Barthet M, Gasmi M, et al. Value of endorectal ultrasonography for diagnosing rectovaginal septal endometriosis infiltrating the rectum. Endoscopy 2005;37:357ŌĆō361PMID : 15824947.


4. Pishvaian AC, Ahlawat SK, Garvin D, Haddad NG. Role of EUS and EUS-guided FNA in the diagnosis of symptomatic rectosigmoid endometriosis. Gastrointest Endosc 2006;63:331ŌĆō335PMID : 16427951.


5. Chung SK, Lee SH, Son BS, et al. Rectal endometriosis that is difficult to differentiate from endoscopically resectable subepitherial lesion. Korean J Gastrointest Endosc 2010;41:319ŌĆō323.
Figure┬Ā2
Endoscopic ultrasonography using a miniprobe showed an indistinctly shaped hypoechoic lesion arising from the muscularis propria layer.
Figure┬Ā3
Pathology findings. (A) Macroscopically, the cut section of sigmoid colon showed an irregularly thickened proper muscle layer and an indented serosal surface with retracted pericolic soft tissue. (B) Microscopically, endometrial glands and stromal cells were embedded in the thickened proper muscle layer (H&E, ├Ś 40; inset, ├Ś 200).
-
METRICS

-
- 0 Crossref
- 0 Scopus
- 9,704 View
- 48 Download
- Related articles
-
Detection of Celiac Ganglia with Radial Scanning Endoscopic Ultrasonography2008 March;23(1)




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print


