 |
 |
| Korean J Intern Med > Volume 27(3); 2012 > Article |
|
Abstract
Constipation is a digestive symptom that is frequently seen in clinical practice. Its prevalence has been reported to be 2% to 20%, depending on geographical region. Despite the rapid development of medical science, systematic studies on constipation have been rarely conducted in Korea. Recently, guidelines on the diagnosis and treatment of functional gastrointestinal disorders, including constipation, were proposed by The Korean Society of Neurogastroenterology and Motility. These guidelines are expected to reflect the current situation regarding treatment of constipation in Korea. In this paper, practical constipation treatment methods that are in current use will be reviewed with reference to these recent guidelines.
Constipation is a digestive symptom that is frequently seen in clinical practice. Its prevalence has been reported to be 2% to 20%, depending on the geographical region [1-3]. Few studies on the prevalence of constipation have been conducted in Korea. A prevalence of 16.5% was reported in one Korean epidemiological study [4]. Constipation may occur because of organic diseases such as endocrine, metabolic or neurological conditions, or colon cancer. However, because most of them appear as functional constipation without an explanatory cause, their management is problematic. In Korea, despite the rapid development of medical science, systematic studies on constipation have been conducted only rarely. Meanwhile, guidelines on the diagnosis [5] and treatment [6] of functional gastrointestinal disorders, including constipation, have recently been proposed by The Korean Society of Neurogastroenterology and Motility (KSNM). Despite the limited data regarding constipation in Korea, these guidelines have been established under the assumption that the results of foreign studies can be applied to the domestic situation, because the difference in the response to drugs among patients of different ethnic backgrounds is insignificant. Furthermore, to overcome limitations, the guidelines refer to data from other Asian countries with a similar epidemiological distribution to that of Korea. To produce guidelines based on a review of domestic and international studies, a consensus among experts was reached using the Delphi method. In addition, a survey via e-mail among doctors in primary and secondary medical institutions was conducted in which the guidelines will be used most frequently, followed by development of clinical treatment guidelines. Therefore, these guidelines are expected to reflect the current situation regarding treatment of constipation in Korea. In this paper, practical constipation treatment methods that are in current use in Korea will be reviewed with reference to these guidelines [6].
To establish proper management, identification of the symptoms and an accurate diagnosis are important. It seems that there is no marked difference in the definition used in Korea and that in other countries [4]. Constipation that is perceived by patients is very comprehensive. It includes various features such as propulsive force during defecation, sense of insufficient defecation, hard stools, a sense of barriers to defecation, longer stay in the bathroom, and decreased frequency of defecation [2,3]. Like other countries, the Korean definition of constipation has been established according to the ROME III criteria proposed in 2006 [7]. In these criteria, functional constipation, excepting that caused by organic factors, is defined as including two or more of the following: 1) straining during at least 25% of defecations; 2) lumpy or hard stools in at least 25% of defecations; 3) sensation of incomplete evacuation for at least 25% of defecations; 4) sensation of anorectal obstruction/blockage for at least 25% of defecations; 5) manual maneuvers to facilitate at least 25% of defecations (e.g., digital evacuation, support of the pelvic floor); and 6) fewer than three defecations per week.
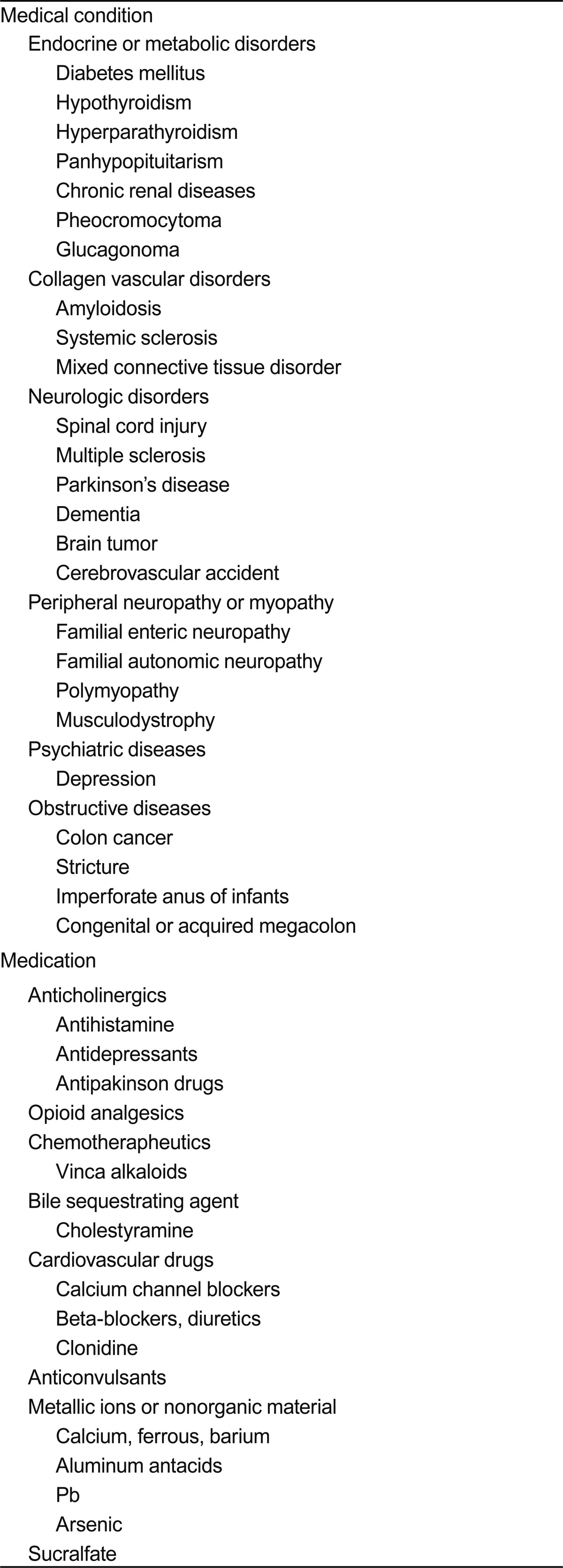
Careful procedures are necessary to exclude secondary constipation. Subjective symptoms can be identified by detailed medical history taking. When patients visit the hospital due to the sudden occurrence of melena, abdominal pain, abdominal distension, and fecal incontinence, an interview appropriate to each situation, including concurrent diseases and current medication, is required. In general, when constipation is associated with identifiable causative factors or systemic diseases, this is called secondary constipation. In particular, the fact that a variety of drugs can cause constipation should be kept in mind. Diseases and drugs frequently related to constipation in Korea are presented in Table 1 [8].
Secondary constipation caused by organic diseases of the colon, rectum, and anus such as colon cancer, stricture, rectocele, and anal fissure is sometimes called organic constipation. In this case, constipation can be cured by treatment of the causative diseases. Other organic forms of constipation are caused by imperforate anus in infants, congenital or acquired megacolon, mucosal prolapse syndrome, and solitary rectal ulcer syndrome.
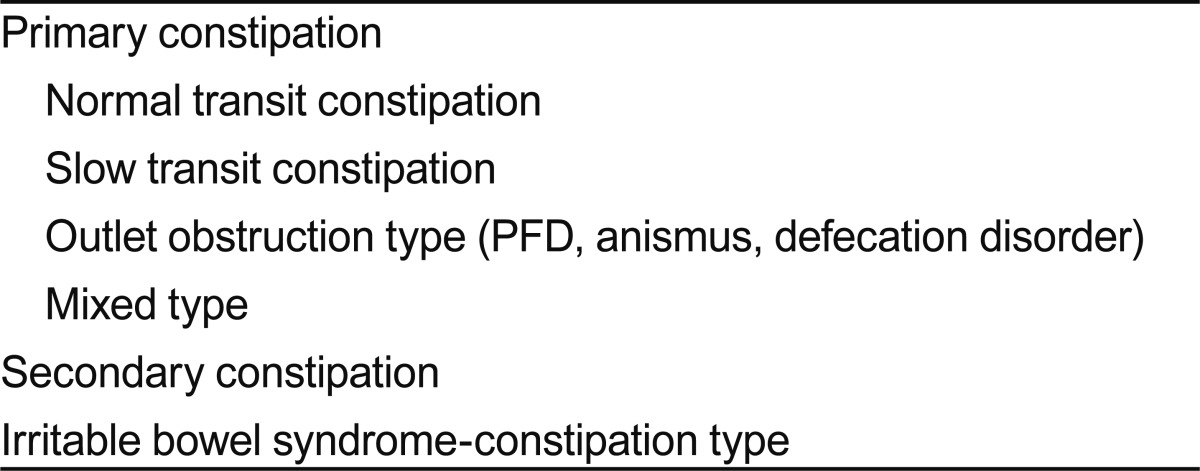
If secondary constipation with known causative factors is excluded, patients are diagnosed with idiopathic or primary constipation. Idiopathic constipation is classified into normal transit, slow transit, and outlet-obstruction-type constipation. Some patients may present with a combination of these subtypes.
Patients with normal-transit constipation frequently complain of infrequent defecation without delayed colon transit, and tend to be unresponsive to laxatives and fiber supplements [9]. These patients may show increased psychosocial distress and misperceive bowel frequency [9,10].
Slow-transit constipation, also called colonic inertia, is usually associated with dysfunction in the enteric plexus or interstitial cells of Cajal, which are the pacemaker cells of gastrointestinal smooth muscle [11]. The typical finding is delayed passage of radiopaque markers through the proximal colon. This is again divided into delayed colonic transit and motility disorder of the colon due to the diffuse whole gastrointestinal tract.
Outlet-obstruction-type constipation is called anismus, defecation disorder, or pelvic floor dyssynergia. In this type, failure in synergic movements among pelvic floor muscles such as puborectalis, external sphincter, and anal internal sphincter muscles causes inadequate defecation [12]. If outlet-obstructive type constipation is suspected, anorectal manometry and defecography may facilitate differentiation of pelvic floor dyssynergia, rectal intussusception, and rectal prolapse.
Irritable bowel syndrome of constipation type or constipation period in mixed type may be another cause of constipation. The classification of constipation according to pathogenesis is summarized in Table 2.
Together with other physical examinations, digital rectal examination is essential. It is important because it is a basic method of identifying organic factors such as rectal cancer, and because it can identify constipation with obstructive defecation by assessing the functions of pelvic floor muscles and internal and external anal sphincter via attempted defecation.
In cases of no response to experiential constipation treatment or patients with warning symptoms such as melena and weight loss, colonoscopy or barium enema should be conducted to exclude colon cancer and other organic diseases.
As mentioned above, the removal of causative factors is critical to the treatment of secondary constipation, which is beyond the scope of this review. Instead, we mainly discuss the treatment of primary constipation.
Dietary control is the most fundamental constipation treatment method. First of all, patients with constipation should have an appropriate water and fiber intake [8]. Although dietary fiber itself has a minimal effect on constipation treatment, it is fermented by normal flora in the colon and induces its proliferation, causing increased stool volume. Dietary control increases defecation frequency and the amount of stool by softening the stools and increasing their volume by combining with water and ions in the colon, leading to improvement of constipation. Usually, a daily fiber intake of 15 to 25 g per day is recommended with sufficient water (1.5 to 2 L) [13]. Dietary fiber is abundant in grains, fruits, and vegetables. If a large amount of fiber is consumed in a short time, complications such as abdominal distension, belching, and diarrhea may occur. In Korea, it has been reported that dietary fiber supplementation reduces symptoms of constipation without side effects and shortens colonic transit time [14-17]. However, Korean studies have been conducted on a small scale and over a short time, therefore, a further large-scale, long-term randomized controlled study is required. Korean clinicians generally agree that the intake of dietary fiber increases the amount of stool and reduces colonic transit time [6]. Therefore, although the effect of dietary fiber on the treatment of constipation is minimal, it could be used as an early treatment because it has the advantages of easy implementation, no adverse effects, and a low cost.
It is important for patients to be in the habit of going immediately to the bathroom for defecation when they want to have a bowel movement. The continuous holding of stools contributes to the vicious cycle of constipation by inhibiting neuromuscular reflex and decreasing sensation [13]. For defecation posture, patients who are unable to sit with their back straight are recommended to adopt the squat position with both legs lifting to the abdomen, or the left decubitus position.
Regular exercise such as walking eases defecation by facilitating colonic motility, but evidence is not insufficient. Physical activities including exercise are known to improve the symptoms of colonic motility in some patients [18-20], but results vary depending among individual patients and according to exercise intensity [21]. In Korea, although there has to-date been no report that exercise improves constipation, short-term, small-scale studies have reported that abdominal massage reduces the symptoms of constipation [22,23]. Domestic clinicians generally agree that exercise improves the symptoms of constipation [6]. Therefore, although the correlation of exercise with constipation is unclear in adult patients, exercise is likely to improve the symptoms of constipation in elderly individuals.
If no response to the aforementioned methods is observed, drug treatment should be considered. Drugs used for the treatment of constipation are classified as bulk-forming, osmotic, stimulant, and other laxatives, according to their mechanism of action [8].
Bulk-forming laxatives are generally considered as a first-line drug. They are not absorbed through the small intestine, and are not degraded by bacteria in the colon. Thus, they can contain water, which in turn increases stool volume in the intestine and the amount of defecation by increasing the level of water in the stool. They are useful for patients who have a sufficient intake of dietary fiber. Brown rice, bran, plant seeds, seaweed, agar, karaya, methylcellulose, and polycarbophil are examples of these agents. Commercially available drugs in Korea include Mutacil®, Agio®, and Sylcon®. However, if these drugs are used in patients with colonic stricture or obstruction, obstructive symptoms may worsen due to increased stool volume. In general, Korean clinicians agree that bulk-forming laxatives are effective in the treatment of constipation [6], although no long-term study is available.
Osmotic laxatives are not absorbed from the colon. They facilitate defecation by softening stools via an increase in water inside the colon. They are classified into salt and hyperosmolar laxatives. Salt laxatives include various Mg salts and phosphate. Mg ions are not absorbed in the intestine; therefore, the gastrointestinal pressure increases due to retention of water. Thus, Mg ions act as a laxative. However, overdose may cause hypermagnesemia; therefore, Mg ions should be administered carefully to patients with renal failure and to children. Although no study of the effect of Mg laxatives on constipation has been conducted in Korean patients with constipation, Mg laxatives have been widely used in such patients elsewhere [24,25], and Korean clinicians generally agree that these are useful for treatment of constipation [6].
Hyperosmolar laxatives include lactulose, sorbitol, lactitol, glycerin, and polyethylene glycol (PEG). These drugs are not absorbed in the intestine and maintain high osmosis in the colon [26-28]. Thus, defecation occurs in a liquid form due to a lack of absorption of water into the body. Korean clinicians generally agree that administration of PEG and various nonabsorbable polysaccharides is effective for treatment of constipation [6]. Hyperosmolar laxatives are likely to be effective drugs that can be safely administered to patients over a long period.
Stimulant laxatives are used if no response to the aforementioned drugs is observed. Although their exact mechanism of action has not been established, they are known to facilitate colonic motility by inhibiting absorption of water and electrolytes and accumulating water and electrolytes [29-32]. Commonly used stimulant laxatives include anthraquinone drugs (e.g., aloe, senna, or cascara) and polyphenol drugs (e.g., bisacodyl or phenolphthalein). Although there is some disagreement among researchers, short-term use of these drugs for several months is generally recommended [13]. In the case of long-term use, loss of water and electrolytes, secondary hyperaldosteronism, steatorrhea, and protein-losing enteropathy may occur. These drugs are abused without prescription in Korea; therefore, they should be prescribed with caution. Although no study of the effect of stimulant laxatives on constipation has been conducted in Korea, they have been used in some patients [6]. In addition, Korean clinicians generally agree that stimulant laxatives are effective in some constipation patients.
Other laxatives include surfactant laxatives and prokinetics. Surfactant laxatives include docusate, castor oil, mineral oil, and dehydrocholic acid. Although they seem to have a stool-softening effect, their effects on chronic constipation are varied [33-37]. No study of the effect of surfactant laxatives on constipation has been conducted in Korea, but they have been widely used. Korean clinicians generally agree that surfactant laxatives are effective in the treatment of constipation [6].
Representative prokinetic drugs for constipation include 5-HT4 receptor agonists such as cisapride, tegaserod, and prucalopride [38-41]. They mediate intestinal peristalsis via 5-HT4 receptors, and stimulate secretion into the intestinal tract. One Korean study reported that cisapride was effective in constipation [42]. Although it is controversial, most of these drugs are not commercially available due to cardiovascular side effects [43]. Even if they are used, it is difficult to achieve efficacy with prokinetics alone in actual clinical practice. In Korea, 5-HT4 receptor agonists have not been available since tegaserod was withdrawn in 2007. New 5-HT4 receptor agonists such as prucalopride, renzapride, and other enterokinetics that are safe and have few side effects have been developed and introduced into clinical practice in Western countries, and are expected to be widely used in Korea in the near future. Korean clinicians generally agree that 5-HT4 receptor agonists are effective in the treatment of constipation [6].
In the case of a lack of response to the aforementioned drugs, suppositories or enema therapy using saline, sodium phosphate, glycerin, and sorbitol may be considered. Types of laxatives according to mechanism of action and typical drugs commercially available in Korea are summarized in Table 3.
If outlet-obstructive type constipation is suspected, it should be diagnosed through an appropriate evaluation such as anorectal manometry [5]. Subsequently, biofeedback therapy leads to improvement of symptoms in about 70% of cases [44-48]. Biofeedback therapy is an educational strategy that recognizes body responses using electrical or mechanical devices [49]. That is, in chronic constipation patients, biofeedback therapy trains the patients to relax the pelvic floor striated muscle during defecation, and to recognize rectal distension caused even by a small amount of stool and to increase abdominal pressure effectively. Biofeedback therapy has been conducted on constipation patients in Korea. Several Korean studies have reported that biofeedback therapy was effective in 70% to 80% of patients with constipation and pelvic floor dysfunction [50-53], and that its efficacy persisted for than 1 year [50]. Korean clinicians generally agree that biofeedback therapy is effective in the treatment of patients with constipation caused by pelvic floor dysfunction [6].
Sacral nerve stimulation (SNS) increases the frequency of defecation and improves constipation symptoms by electrically stimulating the spine and sacral nerve root [54]. The outcomes of this treatment vary [55-58]. Two studies of SNS have been conducted in patients with constipation in Korea, and good treatment outcomes have been reported in patients with slow-transit constipation and impaired rectal sensation [52,59]. Although it is not commonly performed, Korean clinicians agree that SNS is effective in the treatment of constipation [6].
In the case of incurable slow-transit constipation that does not respond to medical treatment, colorectal surgery may be considered [60]. A Korean retrospective study reported relatively high patient satisfaction [61-63]. Korean clinicians generally agree that colorectal surgery is effective in the treatment of some patients with incurable slow-transit constipation [6].
As described above, there are no marked differences in the treatment of constipation between Korea and other countries. However, the number of comprehensive studies on constipation, such as epidemiology or treatment, is currently insufficient. Thus, the development of treatment guidelines specific for Korean patients, that take into consideration ethnicity and regional characteristics, is required. To this end, the KSNM recently proposed domestic guidelines for the diagnosis and treatment of constipation, which will significantly assist clinicians who treat patients with constipation. The constipation study group of the KSNM has been conducting a large clinical cohort study that has comprehensively investigated constipation, including its perception by the Korean population, and its prevalence and treatment, via a nationwide survey.
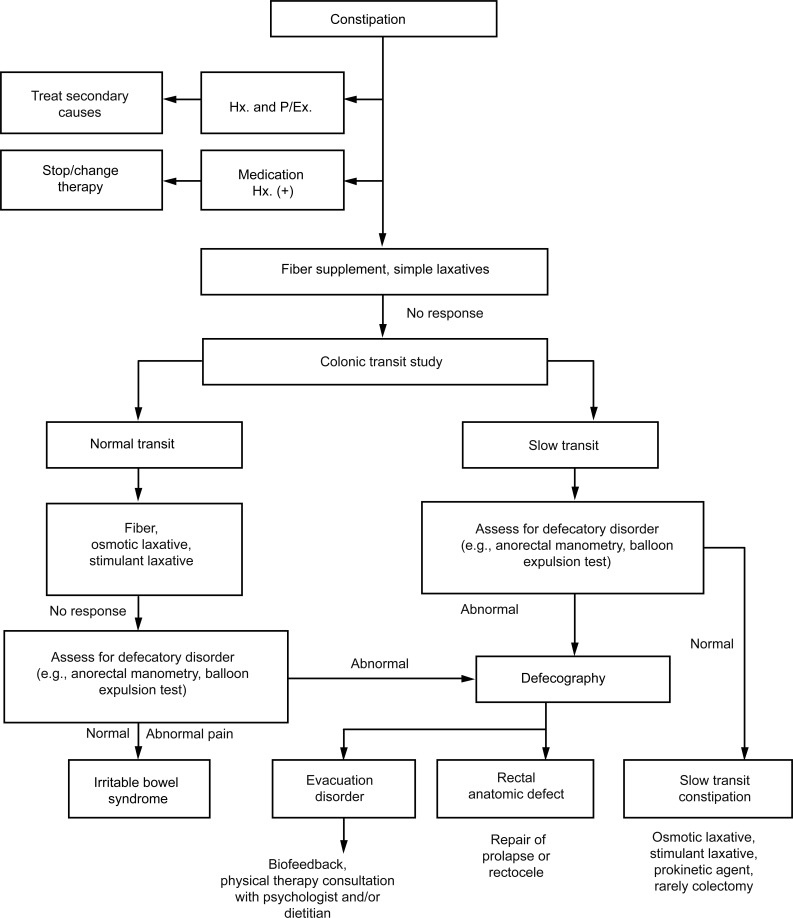
In spite of insufficient data, the practical management algorithm most commonly accepted by Korean clinicians is presented in the Fig. 1. With the interest of clinicians and the efforts of expert groups, the development of guidelines for the treatment of constipation that reflect the domestic situation in Korea is expected to contribute to improvement of the quality of life of patients with constipation.
References
1. Talley NJ, Weaver AL, Zinsmeister AR, Melton LJ 3rd. Functional constipation and outlet delay: a population-based study. Gastroenterology 1993;105:781ŌĆō790PMID : 8359649.


2. Drossman DA, Li Z, Andruzzi E, et al. U.S. householder survey of functional gastrointestinal disorders: prevalence, sociodemography, and health impact. Dig Dis Sci 1993;38:1569ŌĆō1580PMID : 8359066.


3. Johanson JF, Sonnenberg A, Koch TR. Clinical epidemiology of chronic constipation. J Clin Gastroenterol 1989;11:525ŌĆō536PMID : 2551954.


4. Jun DW, Park HY, Lee OY, et al. A population-based study on bowel habits in a Korean community: prevalence of functional constipation and self-reported constipation. Dig Dis Sci 2006;51:1471ŌĆō1477PMID : 16832618.


5. Myung SJ, Lee TH, Huh KC, Choi SC, Sohn CI. Korean Society of Neurogastroenterology and Motility. Diagnosis of constipation: a systematic review. Korean J Gastroenterol 2010;55:316ŌĆō324PMID : 20697191.


6. Park MI, Shin JE, Myung SJ, et al. Guidelines for the treatment of constipation. Korean J Gastroenterol 2011;57:100ŌĆō114PMID : 21350321.


7. Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology 2006;130:1480ŌĆō1491PMID : 16678561.


8. Bouras EP, Tangalos EG. Chronic constipation in the elderly. Gastroenterol Clin North Am 2009;38:463ŌĆō480PMID : 19699408.


9. Wald A, Hinds JP, Caruana BJ. Psychological and physiological characteristics of patients with severe idiopathic constipation. Gastroenterology 1989;97:932ŌĆō937PMID : 2777045.


10. Ashraf W, Park F, Lof J, Quigley EM. An examination of the reliability of reported stool frequency in the diagnosis of idiopathic constipation. Am J Gastroenterol 1996;91:26ŌĆō32PMID : 8561138.

11. He CL, Burgart L, Wang L, et al. Decreased interstitial cell of cajal volume in patients with slow-transit constipation. Gastroenterology 2000;118:14ŌĆō21PMID : 10611149.


12. Rao SS, Welcher KD, Leistikow JS. Obstructive defecation: a failure of rectoanal coordination. Am J Gastroenterol 1998;93:1042ŌĆō1050PMID : 9672327.


14. Han YH, Yon MY, Hyun TS. Effect of prune supplementation on dietary fiber intake and constipation relief. Korean J Community Nutr 2008;13:426ŌĆō438.
15. Huh JW, Park YA, Sohn SK, et al. Effect of yogurt enriched water-soluble fiber on functional constipation. J Korean Soc Coloproctol 2007;23:312ŌĆō320.

16. Kim JY, Kim OY, Yoo HJ, et al. Effects of fiber supplements on functional constipation. Korean J Nutr 2006;39:35ŌĆō43.
17. Kim TI, Park SJ, Choi CH, Lee SK, Kim WH. Effect of ear mushroom (Auricularia) on functional constipation. Korean J Gastroenterol 2004;44:34ŌĆō41PMID : 15266131.

18. Brown WJ, Mishra G, Lee C, Bauman A. Leisure time physical activity in Australian women: relationship with well being and symptoms. Res Q Exerc Sport 2000;71:206ŌĆō216PMID : 10999258.


19. Sandman PO, Adolfsson R, Hallmans G, Nygren C, Nystrom L, Winblad B. Treatment of constipation with high-bran bread in long-term care of severely demented elderly patients. J Am Geriatr Soc 1983;31:289ŌĆō293PMID : 6302153.


20. Hull C, Greco RS, Brooks DL. Alleviation of constipation in the elderly by dietary fiber supplementation. J Am Geriatr Soc 1980;28:410ŌĆō414PMID : 6251128.


21. Sullivan SN, Wong C, Heidenheim P. Does running cause gastrointestinal symptoms? A survey of 93 randomly selected runners compared with controls. N Z Med J 1994;107:328ŌĆō331PMID : 8072729.

22. Kim I, Cho YN. The effects of abdominal meridian massage on constipation in institutionalized psychiatric patients taking antipsychotic drugs. J Korean Acad Adult Nurs 2007;19:809ŌĆō818.
23. Kim MA, Sakong JK, Kim EJ, Kim EH, Kim EH. Effect of aromatherapy massage for the relief of constipation in the elderly. J Korean Acad Nurs 2005;35:56ŌĆō64.

24. Shin EK, Park SJ, Kim KJ, et al. Effect of combination pretreatment of polyethylene glycol solution and magnesium hydroxide for colonoscopy. Korean J Gastroenterol 2010;55:232ŌĆō236PMID : 20389176.


25. Kinnunen O, Salokannel J. Constipation in elderly long-stay patients: its treatment by magnesium hydroxide and bulklaxative. Ann Clin Res 1987;19:321ŌĆō323PMID : 3126699.

26. Freedman MD, Schwartz HJ, Roby R, Fleisher S. Tolerance and efficacy of polyethylene glycol 3,350/electrolyte solution versus lactulose in relieving opiate induced constipation: a double-blinded placebo-controlled trial. J Clin Pharmacol 1997;37:904ŌĆō907PMID : 9505981.


27. Corazziari E, Badiali D, Habib FI, et al. Small volume isosmotic polyethylene glycol electrolyte balanced solution (PMF-100) in treatment of chronic nonorganic constipation. Dig Dis Sci 1996;41:1636ŌĆō1642PMID : 8769292.


28. Andorsky RI, Goldner F. Colonic lavage solution (polyethylene glycol electrolyte lavage solution) as a treatment for chronic constipation: a double-blind, placebo-controlled study. Am J Gastroenterol 1990;85:261ŌĆō265PMID : 2178398.

29. Kienzle-Horn S, Vix JM, Schuijt C, Peil H, Jordan CC, Kamm MA. Efficacy and safety of bisacodyl in the acute treatment of constipation: a double-blind, randomized, placebo-controlled study. Aliment Pharmacol Ther 2006;23:1479ŌĆō1488PMID : 16669963.


30. Delegge M, Kaplan R. Efficacy of bowel preparation with the use of a prepackaged, low fibre diet with a low sodium, magnesium citrate cathartic vs. a clear liquid diet with a standard sodium phosphate cathartic. Aliment Pharmacol Ther 2005;21:1491ŌĆō1495PMID : 15948817.


31. Passmore AP, Wilson-Davies K, Stoker C, Scott ME. Chronic constipation in long stay elderly patients: a comparison of lactulose and a senna-fibre combination. BMJ 1993;307:769ŌĆō771PMID : 8219947.



32. Rouse M, Chapman N, Mahapatra M, Grillage M, Atkinson SN, Prescott P. An open, randomised, parallel group study of lactulose versus ispaghula in the treatment of chronic constipation in adults. Br J Clin Pract 1991;45:28ŌĆō30PMID : 1931536.


33. McRorie JW, Daggy BP, Morel JG, Diersing PS, Miner PB, Robinson M. Psyllium is superior to docusate sodium for treatment of chronic constipation. Aliment Pharmacol Ther 1998;12:491ŌĆō497PMID : 9663731.


34. Castle SC, Cantrell M, Israel DS, Samuelson MJ. Constipation prevention: empiric use of stool softeners questioned. Geriatrics 1991;46:84ŌĆō86PMID : 1718823.

35. Chapman RW, Sillery J, Fontana DD, Matthys C, Saunders DR. Effect of oral dioctyl sodium sulfosuccinate on intake-output studies of human small and large intestine. Gastroenterology 1985;89:489ŌĆō493PMID : 2410320.


36. Fain AM, Susat R, Herring M, Dorton K. Treatment of constipation in geriatric and chronically ill patients: a comparison. South Med J 1978;71:677ŌĆō680PMID : 78527.


37. Hyland CM, Foran JD. Dioctyl sodium sulphosuccinate as a laxative in the elderly. Practitioner 1968;200:698ŌĆō699PMID : 4870204.

38. Tack J, van Outryve M, Beyens G, Kerstens R, Vandeplassche L. Prucalopride (Resolor) in the treatment of severe chronic constipation in patients dissatisfied with laxatives. Gut 2009;58:357ŌĆō365PMID : 18987031.


39. Camilleri M, Kerstens R, Rykx A, Vandeplassche L. A placebo-controlled trial of prucalopride for severe chronic constipation. N Engl J Med 2008;358:2344ŌĆō2354PMID : 18509121.


40. Fried M, Johanson JF, Gwee KA, Wagner A, Pecher E, Rueegg P. Efficacy of tegaserod in chronic constipation in men. Am J Gastroenterol 2007;102:362ŌĆō370PMID : 17156137.


41. Tack J, Muller-Lissner S, Bytzer P, et al. A randomised controlled trial assessing the efficacy and safety of repeated tegaserod therapy in women with irritable bowel syndrome with constipation. Gut 2005;54:1707ŌĆō1713PMID : 16020489.



42. Yang US, Cho JH, Koo JY, et al. The effect of cisapride tartrate in patients with functional dyspepsia and functional constipation. Korean J Gastrointest Motil 2001;7:36ŌĆō46.
43. Loughlin J, Quinn S, Rivero E, et al. Tegaserod and the risk of cardiovascular ischemic events: an observational cohort study. J Cardiovasc Pharmacol Ther 2010;15:151ŌĆō157PMID : 20200325.


44. Chiarioni G, Salandini L, Whitehead WE. Biofeedback benefits only patients with outlet dysfunction, not patients with isolated slow transit constipation. Gastroenterology 2005;129:86ŌĆō97PMID : 16012938.


45. Mason HJ, Serrano-Ikkos E, Kamm MA. Psychological state and quality of life in patients having behavioral treatment (biofeedback) for intractable constipation. Am J Gastroenterol 2002;97:3154ŌĆō3159PMID : 12492203.


46. Chiotakakou-Faliakou E, Kamm MA, Roy AJ, Storrie JB, Turner IC. Biofeedback provides long-term benefit for patients with intractable, slow and normal transit constipation. Gut 1998;42:517ŌĆō521PMID : 9616314.



47. Rao SS, Welcher KD, Pelsang RE. Effects of biofeedback therapy on anorectal function in obstructive defecation. Dig Dis Sci 1997;42:2197ŌĆō2205PMID : 9398795.


48. Enck P. Biofeedback training in disordered defecation: a critical review. Dig Dis Sci 1993;38:1953ŌĆō1960PMID : 8223066.


49. Emmanuel AV, Kamm MA. Response to a behavioural treatment, biofeedback, in constipated patients is associated with improved gut transit and autonomic innervation. Gut 2001;49:214ŌĆō219PMID : 11454797.



50. Lee BH, Kim N, Kang SB, et al. The long-term clinical efficacy of biofeedback therapy for patients with constipation or fecal incontinence. J Neurogastroenterol Motil 2010;16:177ŌĆō185PMID : 20535349.



51. Jung KW, Myung SJ, Byeon JS, et al. Response to biofeedback therapy for patients with rectal hyposensitivity. Intest Res 2008;6:56ŌĆō69.
52. Chang HS, Myung SJ, Yang SK, et al. Electrical stimulation effect in constipated patients with impaired rectal sensation. Korean J Gastrointest Motil 2002;8:160ŌĆō166.

53. Jeong JH, Choi JS, Seo YJ, Kim JH. Biofeedback therapy in patients with nonrelaxing puborectalis syndrome: are there differences of therapeutic effect according to methods of diagnosis? J Korean Soc Coloproctol 2001;17:26ŌĆō32.
54. Pescatori M. Systematic review of sacral nerve stimulation for faecal incontinence and constipation (Br J Surg 2004; 91:1559-1569). Br J Surg 2005;92:379. PMID : 15739252.

55. Holzer B, Rosen HR, Novi G, et al. Sacral nerve stimulation in patients with severe constipation. Dis Colon Rectum 2008;51:524ŌĆō529PMID : 18322757.


56. Malouf AJ, Wiesel PH, Nicholls T, Nicholls RJ, Kamm MA. Short-term effects of sacral nerve stimulation for idiopathic slow transit constipation. World J Surg 2002;26:166ŌĆō170PMID : 11865344.


57. Kenefick NJ, Nicholls RJ, Cohen RG, Kamm MA. Permanent sacral nerve stimulation for treatment of idiopathic constipation. Br J Surg 2002;89:882ŌĆō888PMID : 12081738.


58. Ganio E, Masin A, Ratto C, et al. Short-term sacral nerve stimulation for functional anorectal and urinary disturbances: results in 40 patients: evaluation of a new option for anorectal functional disorders. Dis Colon Rectum 2001;44:1261ŌĆō1267PMID : 11584196.


59. Song HK, Myung SJ, Yang SK, et al. Noninvasive sacral nerve stimulation for idiopathic slow transit constipation: short term clinical and physiologic effects. Korean J Neurogastroenterol Motil 2003;9:134ŌĆō141.
60. Knowles CH, Dinning PG, Pescatori M, Rintala R, Rosen H. Surgical management of constipation. Neurogastroenterol Motil 2009;21(Suppl 2):62ŌĆō71PMID : 19824939.


61. Lee HC, Hong SN, Lee JH, et al. Clinical features and functional outcome of the patients with idiopathic chronic constipation who underwent surgical treatment. Korean J Gastrointest Motil 2001;7:204ŌĆō215.
62. Nam KH, Sohn SK. Clinical results of subtotal colectomy in chronic constipation patients. J Korean Soc Coloproctol 2000;16:395ŌĆō401.
63. Lim SW, Oh SH, Lee WY. Clinical analysis of total colectomy for chronic idiopathic constipation. J Korean Soc Coloproctol 2000;16:150ŌĆō155.
-
METRICS

- Related articles
-
Treatment patterns of knee osteoarthritis patients in Korea2019 September;34(5)
Practical management of peripartum cardiomyopathy2017 May;32(3)
Appropriate candidates for statin use in heart failure2014 November;29(6)
Newer treatments for advanced hepatocellular carcinoma2014 March;29(2)
The Current Practice of Skin Testing for Antibiotics in Korean Hospitals2010 June;25(2)




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print


