 |
 |
| Korean J Intern Med > Volume 22(1); 2007 > Article |
|
Abstract
Background
Volatile organic compounds (VOCs) in concentrations found in both the work and home environments may influence lung function. We investigated the prevalence of airway responsiveness in workers exposed to VOCs.
Methods
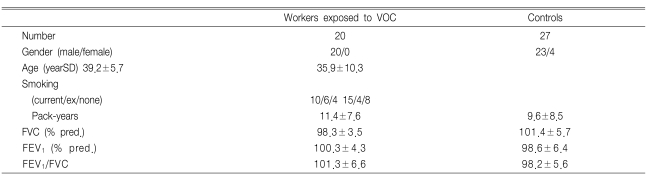
We used allergic skin tests, nonspecific airway hyperresponsiveness testing and questionnaires to study twenty exposed workers and twenty-seven control subjects. Atopy was defined as a reactor who showed >3+ response to one or more allergens on the skin prick tests. Airway hyperresponsiveness (BRindex) was defined as log [% fall of FEV1/ log (last concentration of methacholine) +10].
Results
The VOC exposed workers, in comparison with the control subjects, tended to have a higher BRindex (1.19±0.07 vs. 1.15±0.08, respectively). Workers exposed to VOCs with atopy or smoker, as compared with the workers exposed to VOCs with non-atopy and who were non-smokers and the control subjects with non-atopy and who were non-smokers, had a significantly higher BRindex (1.20±0.05 vs. 1.14±0.06 vs. 1.10±0.03, respectively p<0.05). The BRindex was not correlated with atopy, the smoking status or the duration of VOC exposure.
Organic chemicals are ubiquitous indoors, where they are released from furnishings and equipment, construction materials and consumer and office products1). Because these sources of organic chemicals are not always well ventilated, volatile organic compounds (VOC) are generated and trapped indoors and so this causes higher indoor levels than are found outdoors. Recently, there have been concerns raised about the adverse health effects of such exposure.
Hundreds of organic chemicals have been identified in indoor air1). Although many of these agents are also released by outdoor sources such as chemical plants, these indoor sources have been shown to be responsible for the better part of a person's exposures to most organic chemicals1).
Despite the potential risks of the organic chemicals in indoor air, there have been few studies concerned with specific exposure-disease associations, largely because of the difficulty in characterizing the exposures and identifying the effects of complex mixtures of compounds in indoor and outdoor air. There have also been a few studies2-6) that have shown specific exposure-disease associations in the occupational environment.
The VOCs at concentrations found in both work and home environments may influence lung function and they are probably of importance as bronchial irritants7).
The aim of this study was to investigate airway hyperresponsiveness (AHR) in workers who were exposed to VOCs at one petrochemical plant in Korea.
The subjects consisted of twenty workers who were exposed to VOCs and twenty-seven non-exposed control subjects. The exposed workers were working at a petrochemical plant at the time of the study. The non-exposed control subjects were watched over the VOC factory. The exposed workers and non-exposed control subjects were randomly selected. The ambient air concentrations of VOCs were monitored as part of an epidemiological survey. The subject's symptoms included cough, wheezing, shortness of breath, chest tightness, stuffiness, coryza and sneezing that occurred at work, during the evening or at night. All the subjects completed an interview about their clinical and occupational history. All subjects were free of respiratory infection at the time of the interview. None of the subjects took anti-histamine, cromolyn, theophylline or symphathomimetics within 72 hours of the challenge tests.
A questionnaire for symptoms and medications was given and spirometry was performed for each subject. The skin prick tests and methacholine provocation tests were then done.
Each subject was interviewed by trained field investigators by using a structured questionnaire. We obtained data on respiratory symptoms, a detailed work history that included previous employment, and the medical history that included the presence of atopy and the subject's smoking habits.
Spirometry was performed with a SensorMedics 2200 spirometer (Cardiopulmonary care companyTM, Yorba Linda, California). Baseline measurements of vital capacity and FEV1 (forced expiratory volume in one second) were selected according to the American Thoracic Society criteria8) and reference values were taken from Choi et al.9).
Allergy skin prick tests were performed with nine common allergen extracts [Dermatophagoides farinae, Dermatophagoides pteronyssinus, aspergillus spp, alder, rye, mugwort, ragweed, Blatella germinica, cat fur and histamine (1 mg/mL, Bencard, Bradford UK) mixed with saline. The reactions were read 15 minutes later. When the wheal size was equal to or greater than that of histamine (the positive control) and the erythema size was equal or greater than that of histamine, it was read as 3+. Atopy was defined as a reactor who showed >3+ response to one or more allergens on the skin prick tests10).
Methacholine challenge tests were carried out by the method described by Chai et al. with some modifications11), and the results were expressed as the PC20 [defined as a provoking dose of methacholine causing a 20% fall in the FEV1] in non-cumulative units. Nebulized methacholine dilutions varying from 0.075 to 25 mg/mL were administered. The FEV1 was measured 30, 60 and 90 seconds after nebulization until a 20% decrement in the FEV1 was demonstrated. The AHR was estimated as the concentration dose that provoked a 20 percent decrease of the FEV1. The PC20 level was obtained from the dose-response curve. The BRindex, as described by O'Connor et al.12) with some modifications13), was defined as log [(% fall of FEV1)/log (last concentration of methacholine) +10].
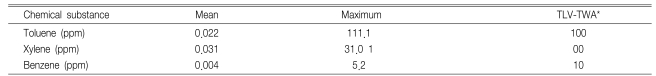
The ambient air concentrations of toluene, xylene and benzene were measured when manufacturing was taking place at the workplace14).
All the data was analyzed using SPSS version 10.0 for Windows. The data are expressed as mean standard deviation (SD). Statistical analysis was performed by the Mann-Whitney U test. Spearman's correlations were used were appropriate. A p-value of <0.05 was considered significant.
The characteristics of the subjects are given in Table 1. The mean ambient air concentrations of VOCs were under the recommended levels (Table 2). The mean (SD) duration of exposure of workers to VOCs was 9.1±5.3 years. The mean duration of respiratory symptoms for the workers exposed to VOCs was 7.1±5.2 years.
Four of twenty workers and seven of twenty-seven control subjects had atopy. Differences for the prevalence of atopy were not noted between the workers exposed to VOCs and the control subjects.
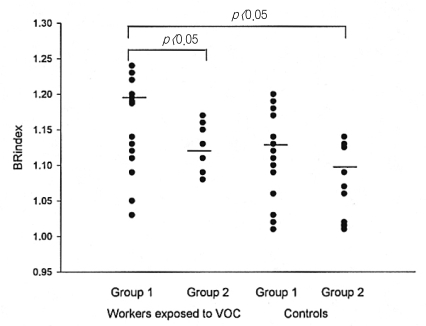
Four workers (20.0%) were shown to have respiratory symptoms. The VOC exposed workers, in comparison with the control subjects, tended to have a higher BRindex (1.19±0.07 vs. 1.15±0.08, respectively, Figure 1). There were no differences in the prevalence of nasal symptoms between the exposed workers and the control subjects. There were no differences of the BRindex between the atopy subjects and the non-atopy subjects (1.21±0.05 vs. 1.19±0.06, respectively), between the subjects with ≥10 year exposure and the subjects with < 10 year exposure (1.16±0.07 vs. 1.19±0.09, respectively), and between the smokers and non smokers (1.17±0.05 vs. 1.16±0.04, respectively, Figure 2). The workers exposed to VOCs and with atopy or smoking (n=13), had a significantly higher BRindex (1.20±0.05 vs. 1.14±0.06 vs. 1.10±0.03, respectively, Figure 2) in comparison with the VOC workers (n=7) and the control subjects with non-atopy and who didn't smoke (n=9).
These data showed that workers exposed to VOCs with atopy or that were smokers had a higher AHR in comparison to the non-atopy, non-smoking VOC exposed workers.
The relationship between allergens in the indoor environment and asthma has been extensively studied and recent studies have suggested the possibility of the role of chemical pollutants for the genesis of asthma in the occupational environment.
The organic chemicals found in indoor air can be grouped by their range of boiling points as volatile (0 to 240℃), semivolatile (240 to 380℃), and particulate (over 380℃)15, 16). The volatile and semivolatile organic chemicals are most relevant to human health. VOCs exist as vapors over the normal range of air temperature and pressures, whereas semivolatile organic chemicals are liquids or solids, but they also evaporate slowly17).
Despite the potential risks of the organic chemicals in the work environment, few studies2, 18) have shown specific disease-exposure associations.
VOCs at concentrations found in both work and home environments may influence the functioning of lungs and they are probably important as bronchial irritants7). Yet the residential indoor and outdoor VOC concentrations measured in Seoul were significantly higher than those found in Asan, suggesting that the VOC levels are higher in polluted area in comparison with the less polluted area19).
Indoor exposure to tobacco smoke, some VOCs and various combustion products (either by using unvented stoves or from outdoor sources) can be related to asthmatic symptoms. In this study, exposed workers with smoking or atopy had a higher BRindex, suggesting that smoking is an important additive factor to VOCs in relation to AHR. In some susceptible individuals, the development of respiratory hypersensitivity or the elicitation of asthmatic symptoms may also be related to the indiscriminate use of different household products and then this is followed by exposure to such compounds as diisocyanate, organic acid anhydrides, formaldehyde, styrene and hydroquinone20). The VOC emissions from solvent-based paints might contribute to the development of respiratory symptoms and airway irritation7). There are probably some patients with an increased sensitivity to paint fumes who would derive a useful symptomatic benefit from using VOC-free paint20). Some of the VOCs emitted by rape-seed oil have the potential to be allergens/irritants21). In this study, there was no difference of AHR between the workers exposed to VOCs and the control subjects. Further, there was no AHR difference between the atopy and non-atopy workers exposed to VOC. The absence of AHR differences maybe due to the study population and the low VOC concentrations, as compared to the previous study of Ware et al23). Further studies with larger subject pools are needed to clarify the relation between workers exposed to VOCs and the control subjects. Although there were no differences of AHR between the workers exposed to VOCs with atopy and the workers exposed to VOCs with smoking and the control subjects, the workers with atopy or smoking showed increased AHR, suggesting that VOCs might contribute as an aggravating factor of AHR.
Exposure to chemical emissions from indoor paint is related to asthma, and some VOCs may cause inflammatory reactions in the airways18). Significant relationships have been noted between nocturnal breathlessness and the presence of wall-to-wall carpets, and the indoor concentrations of CO2, formaldehyde and VOCs. AHR is related to the indoor concentration of limonene, which is the most prevalent terpene. Variability in the peak expiratory flow rates is related to two other terpenes: alpha-pinen and delta-karen. This suggests that indoor VOCs and formaldehyde may cause asthma-like symptoms22). The incidence of chronic respiratory symptoms is also positively associated with the concentrations of volatile organic compounds, considering that exposure to volatile organic compounds, including the emissions from chemical manufacturing plants, is associated with increased rates of chronic respiratory symptoms that are characteristic of reactive airways23). For improving the management of asthma and to counteract the increasing frequency of asthma, the significance of the work environment can not be neglected18).
However, because of the selection effects, the results of cross-sectional studies on respiratory symptoms in relation to occupational exposure to VOC emissions may be inconclusive. Despite the small size of the worker groups in this study, significant differences in the AHR of the workers exposed to VOCs with atopy or smoking were detected, and this suggests that VOCs may increase AHR. Further prospect studies with larger populations of workers should be done.
In the present study, any association between VOCs and AHR was not seen, but when this was adjusted for smoking or atopy, the association with VOC exposure was evident. Therefore, there is a need to decrease people's exposure to VOCs and to improve the air supply in the work environment. Improved work environment can also be achieved by selecting proper building materials and paying close attention on the various options and choices when constructing a building. The emission of VOCs should be as low as reasonably achievable to minimize the asthma-related symptoms that are due to polluted air in the work environment.
In conclusion, this study indicated that the workers exposed to VOCs with atopy or that are smokers have increased AHR as compared to workers exposed to VOCs with non-atopy and that are non-smokers, in one Korean petrochemical plant. Therefore, volatile organic chemicals should be well ventilated during use in occupational and home environments to reduce the occurrence of asthma-related symptoms.
Notes
This work was supported by a grant from the Korea Health 21 R&D Project, Ministry of Health and Welfare, Republic of Korea (01-PJ3-PG6-01GN04-003 and 0412-CR03-0704-0001).
References
1. Youngson C, Nurse C, Yeger H, Cutz E. Oxygen sensing in airway chemoreceptors. Nature 1993. 365:153–155PMID : 8371757.


2. Beach JR, Raven J, Ingram C, Bailey M, Johns D, Walters EH, Abramson M. The effects on asthmatics of exposure to a conventional water-based and a volatile organic compound-free paint. Eur Respir J 1997. 10:563–566PMID : 9072985.

3. Wieslander G, Norback D, Edling C. Airway symptoms among house painters in relation to exposure to volatile organic compounds (VOCS): a longitudinal study. Ann Occup Hyg 1997. 41:155–166PMID : 9155237.


4. Dales R, Raizenne M. Residential exposure to volatile organic compounds and asthma. J Asthma 2004. 41:259–270PMID : 15260458.


5. Krzyzanowski M, Quakenboss JJ, Lebowitz MD. Chronic respiratory effects of indoor formaldehyde exposure. Environ Res 1990. 52:117–125PMID : 2394203.


6. Rumchev KB, Spickett JT, Bulsara MK, Phllips MR, Stick SM. Domestic exposure of formaldehyde significantly increases the risk of asthma in young children. Eur Respir J 2002. 20:403–408PMID : 12212974.


7. Harving H, Dahl R, Molhave L. Lung function and bronchial reactivity in asthmatics during exposure to volatile organic compounds. Am Rev Respir Dis 1991. 143:751–754PMID : 2008987.


8. American Thoracic Society. Lung function testing: selection of reference values and interpretative strategies. Am Rev Respir Dis 1991. 144:1202–1218PMID : 1952453.
9. Choi IS, Greville HW, Park KO. Addition of peak expiratory flow rate to the selection criteria of the representative spirometric result. Chonnam J Med Sci 1990. 3:23–28.
10. Crockcroft DW, Murdock KY, Berscheid BA. Relationship between atopy and bronchial responsiveness to histamine in a random population. Ann Allergy 1984. 53:26–29PMID : 6742522.

11. Chai H, Farr RS, Froehlich LA, Mathison DA, Mclean JA, Rosenthal RR, Scheffer AL, Spector SL, Townley RG. Standardization of bronchial inhalation challenge procedures. J Allergy Clin Immunol 1975. 56:323–327PMID : 1176724.


12. O'Connor G, Sparrow D, Taylor D, Segal M, Weiss S. Analysis of dose-response curves to methacholine: an approach suitable for population studies. Am Rev Respir Dis 1987. 136:1412–1417PMID : 3318599.


13. Burrow B, Sears MR, Flannery EM, Herbison GP, Holdaway MD. Relationships of bronchial responsiveness assessed by methacholine to serum IgE, lung function, symptoms and diagnoses in 11-year old New Zealand children. J Allergy Clin Immunol 1992. 90:376–385PMID : 1527320.


14. American Conference of Government Industrial Hygiensts. Threshold limit values (TLVs) for chemical substances and physical agents and biological exposure indices 1995. ACGIH.
15. Wolkoff P. Volatile organic compounds-Sources, measurements, emissions, and the impact on indoor air quality. Indoor Air 1995. 3:71–73.

16. Otto DA, Hudnell HK, House DE, Molhave L, Counts W. Exposure of humans to a volatile organic mixture: I. behavioral assessment. Arch Environ Health 1992. 47:23–30PMID : 1539999.


17. Samet JM, Utell MJ. In: Fishman AP, Elias JA, Fishman JA, Grippi MA, Kaiser LR, Senior RM, eds. Indoor and outdoor air pollution. Fishman's pulmonary diseases and disorders 1998. New York: McGraw-Hill, 941–963.
18. Wieslander G, Norback D, Bjornsson E, Janson C, Boman G. Asthma and the indoor environment: the significance of emission of formaldehyde and volatile organic compounds from newly painted indoor surfaces. Int Arch Occup Environ Health 1997. 69:115–124PMID : 9001918.


19. Son B, Breysse P, Yang W. Volatile organic compounds concentrations in residential indoor and outdoor and its personal exposure in Korea. Environ Int 2003. 29:79–85PMID : 12605940.


20. Becher R, Hongslo JK, Jantunen MJ, Dybing E. Environmental chemicals relevant for respiratory hypersensitivity: the indoor environment. Toxicol Lett 1996. 86:155–162PMID : 8711767.


21. Butcher RD, Goodman BA, Deighton N, Smith WH. Evaluation of the allergic/irritant potential of air pollutants: detection of proteins modified by volatile organic compounds from oilseed rape (Brassica napus ssp. oleifera) using electrospray ionization-mass spectrometry. Clin Exp Allergy 1995. 25:985–992PMID : 8556570.


Figure 1
BRindexs between the workers exposed to volatile organic compounds and the control subjects.
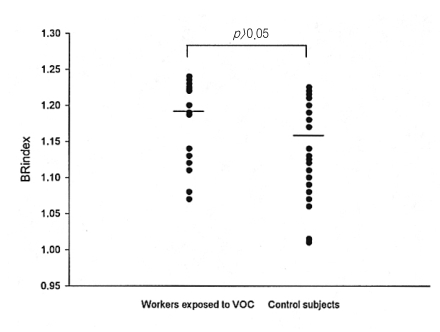
Figure 2
BRindexs among the atopy or smoking group of workers exposed to volatile organic compounds (Group 1), the non-atopy and non-smoking group of workers (Group 2) exposed to volatile organic compounds and the control subjects.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



