INTRODUCTION
Episodic angioedema with eosinophilia (EAE), originally described by Gleich et al. in 19841), is a syndrome characterized by recurrent episodes of angioedema, fever, leukocytosis, eosinophilia, elevated serum IgM, increased body weight, and a benign clinical course lacking any internal organ involvement. Many other cases have been detected since this initial report, and this syndrome has been recognized as a distinct clinical entity2, 3). More than 40 cases with symptomatic presentations and laboratory findings similar to EAE have been reported, but these cases have not involved recurrent attacks, and thus have been subsequently designated as nonepisodic angioedema with eosinophilia (NEAE)4-8). The majority of these NEAE cases have been reported in Japanese patients, with the exception of three cases reported in the Korean literature7-9). No cases have yet been reported in Western populations. This ethnic or regional distribution may be an important characteristic of NEAE. In this paper, we describe a patient whose clinical and laboratory features were similar to those observed in previous cases of NEAE, and also present our review of cases thus far reported in Korea.
CASE REPORT
A 26-year-old Korean woman presented with edema of her hands and lower legs, which had developed 2 weeks prior to her hospital visit. Her body weight had increased by 2 kg over those 2 weeks, and this was her first episode of the reported symptoms. The edema was distributed symmetrically on both of the patient's upper and lower extremities, and was pitted. She denied any febrile sensation and had a pruritic rash on her lower legs (Figure 1A-1C), and had also experienced mild joint pain in both knees 1 week after the onset of the edema. Her family and past medical histories, including any allergic diseases, were unremarkable. She also denied taking any drugs, including Oriental medications, with the exception of one acetaminophen tablet (300 mg) 1 week prior to the onset of edema. Her symptoms did not appear to be related to her menstrual cycle.
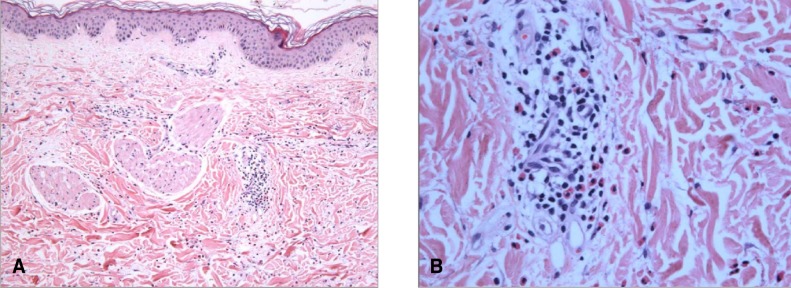
Laboratory tests revealed leukocytosis (12,250/mm3; normal range: 4,000-10,000/mm3) with 51.5% eosinophils (normal range: 0~7%) in the peripheral blood. The eosinophil count was 6,300/mm3. Serum IgE had increased to 1,423 IU/mL (normal range: 0-170 IU/mL), but IgA, IgG, and IgM levels were all within normal limits. Antinuclear antibody was negative, as were stool ova and serum antibodies to parasites. No clinical findings were suggestive of autoimmune disease or parasite infestation. No abnormal findings were observed in the serum chemistry that would be reflective of renal or hepatic dysfunction. No proteinuria was detected. The rash on the patient's lower legs was examined histologically, and identified as perivascular eosinophil infiltration (Figure 2). Lymphocyte phenotyping was conducted, but did not indicate the presence of any abnormal lymphocyte clones.
We diagnosed the patient with NEAE, and prescribed an oral antihistamine to control the pruritus. One week after the patient began taking antihistamines, the edema and rash began to evidence improvements. The knee arthralgia also clearly improved. The eosinophil count decreased to 1,530/mm3 after 2 weeks and to 736/mm3 after 8 weeks. The patient was free of symptoms at 4 months, and had an eosinophil count of 550/mm3. We followed the patient for 18 months, and observed no recurrence of either the symptoms or the eosinophilia (the eosinophil count was 180/mm3).
DISCUSSION
Our patient presented with eosinophilia with angioedema localized to the upper and lower extremities, and evidenced features typical of the NEAE cases thus far reported in Japan. That is, the patient was a young female exhibiting a mild weight gain, and her condition lacked internal organ involvement, improved without corticosteroids, involved no increase in IgM levels, and did not recur over the course of 18 months. The skin biopsy indicated perivascular eosinophil infiltration.
EAE is characterized by recurrent edema and requires the administration of corticosteroids, and has also been reported principally in Europe and the United States. However, in Japan and Korea, more than 40 cases have been reported with clinical symptoms similar to those observed in EAE, but without recurrent episodes; these patients recovered without corticosteroid treatment4-8). Chikama et al. first gave this distinct form of EAE the designation NEAE4), which has been loosely identified as a less severe form of EAE6). The most notable aspect of NEAE is the absence of recurrence, but several other differences also exist with regard to the clinical features of NEAE and EAE. One of these differences is the distribution of the edema. In NEAE, the angioedema is normally localized to the hands and the proximal portion of the lower legs, as in the present case, whereas in EAE, the angioedema frequently extends farther down the extremities, sometimes including the face10). The edema in EAE is attended by a substantial increase in body weight. An increase in serum IgM levels is also normally detected in cases of EAE, but is seldom observed in NEAE6, 10). Almost all EAE patients require corticosteroid therapy, whereas spontaneous remission frequently occurs in patients suffering from NEAE. Additionally, all NEAE patients thus far have been young females, as in the case described herein4-8).
The pathogenesis of EAE and NEAE remains to be thoroughly elucidated. The cause of the sudden increase of eosinophils remains unknown, as with idiopathic hypereosinophilic syndrome. The identification of abnormal clonal CD3- CD4+ cells in the blood of some EAE sufferers11) indicates that EAE and NEAE may be, in some if not all patients, a disease that involves abnormal T cell clones, similarly to the lymphocytic variant of hypereosinophilic syndrome12). The predilection to affect the skin with an absence of internal organ involvement in EAE and NEAE is also a clinical feature reminiscent of the lymphocytic variant of hypereosinophilic syndrome12). In the case described herein, we conducted lymphocyte phenotyping in order to determine the presence of any aberrant clonal lymphocytes, as has been observed in cases of the lymphocytic variant of hypereosinophilic syndrome13). However, our results in this regard were negative. The angioedema of EAE and NEAE is likely associated with a temporal increase in the vascular permeability of local capillaries via some mediators, including antiendothelial cell antibodies and cytokines3, 14-16). Several reports have shown that histamine levels are within normal limits, and that IL-1, IL-5, and IL-6 generated by monocytes, endothelial cells, T cells, and eosinophils increase during the acute phase of EAE3, 5, 11, 15, 16). According to a recent report, IL-5 levels were determined to be lower, and TNF-╬▒levels were higher in the acute phase of NEAE than in the acute phase of EAE. Thus, the cytokine profile may be related with the existence or absence of recurrent attacks5).
Recently, several cases of EAE and NEAE have been reported in Korea7-9, 17). Table 1 shows these six cases of EAE and NEAE, including the case described in this paper. Cases 1, 2, and the present case were readily diagnosed as NEAE, whereas cases 3 and 5 were thought to be EAE. In case 4, certain aspects, such as the elevated serum IgM level and the necessity for corticosteroid therapy to control the symptoms, supported a diagnosis of EAE. However, the presence of other aspects, including the fact that it occurred in a young female, the absence of weight gain, and the absence of a previous episode or recurrence, was suggestive of NEAE. This series of NEAE and EAE case reports from Korea demonstrates that NEAE and EAE are not rare diseases within the Korean population, and also suggests that NEAE may have a racial predisposition toward Asian populations.
In this work, we have described the case of a Korean patient with NEAE and have reviewed five other cases of NEAE and EAE occurring in Korean patients. As in the Japanese population, NEAE is not an uncommon disease within the Korean population. Further studies will be required in order to clarify the pathogenesis of NEAE.





 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print





