INTRODUCTION
Masked hypertension (MH) is defined as the presence of normal office blood pressure (BP) but high out-of-office BP, as determined by 24-hour ambulatory blood pressure monitoring (ABPM) or home BP monitoring [
1]. As MH could also refer to those individuals not taking antihypertensive drugs, high out-of-office BP with normal office BP in patients on antihypertensive therapies, which was first described 10 years ago, was later renamed as masked uncontrolled hypertension (MUCH) [
2]. MH is known to increase the risk of cardiovascular diseases as it is often undetected and untreated [
3]. Previous studies on MH included patients with MUCH and did not distinguish cardiovascular risks between patients receiving antihypertensive therapies and those not receiving antihypertensive therapies [
4–
6]. Other studies previously reported significantly higher cardiovascular risk in patients with MUCH than in those with controlled hypertension [
7–
9]. The prognostic value of MUCH is not yet clear, but it is inseparable from MH in terms of increased cardiovascular risk. In outpatient department settings, where office BP remains the main BP assessment tool, no effective indicator has been widely used to detect MUCH, and therefore, it is difficult to suspect in daily practice. It is desirable to recognize clinical features strongly related to the presence of MUCH and to utilize these features as an effective screening tool for MUCH that can be easily availed in the outpatient setting. In this study, we investigated the clinical characteristics of MUCH and identified significant predictors for the presence of MUCH, using which we developed a prediction model for MUCH in patients who were treated with antihypertensive drugs.
METHODS
Study design and setting
Cross-sectional study data were obtained from the nationwide Korean ABPM (Kor-ABP) Registry for Evaluation of the Prognostic Threshold in Hypertension, organized by the Korean Society of Hypertension. This prospective multicenter cohort included patients who underwent 24-hour ABPM to evaluate high BP. The Kor-ABP registry involved outpatient clinics in 27 tertiary and secondary hospitals between August 2009 and December 2016 [
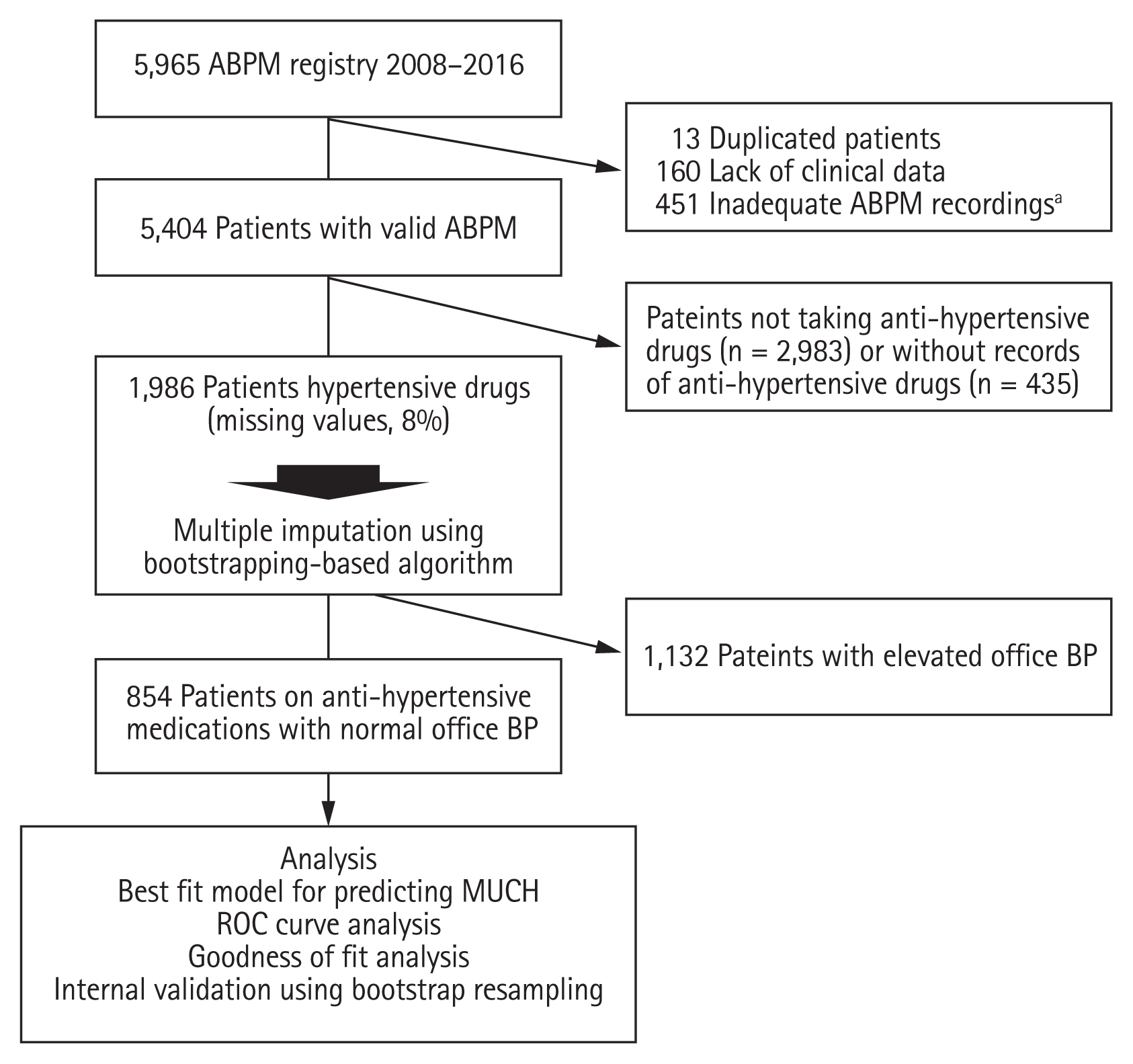
10]. Treatment and drug administration were performed at the discretion of physicians for patients with hypertension, and all investigators were cardiologists who were experts on hypertension and clinical cardiology. Among the initially enrolled 5,965 patients who had undergone 24-hour ABPM, 5,404 patients had valid 24-hour ABPM data. Of these, 1,986 patients were treated with antihypertensive drugs. A total of 1,132 patients with elevated office BP (systolic blood pressure [SBP] ≥ 140 mmHg and/or diastolic blood pressure [DBP] ≥ 90 mmHg) were excluded. Therefore, 854 patients treated with antihypertensive drugs with normal office BP (SBP < 140 mmHg and/or DBP < 90 mmHg) were included in the final analysis, and we classified the patients into groups according to BP characteristics obtained from 24-hour ABPM as the MUCH and controlled hypertension groups (
Fig. 1).
The study protocol complied with the Declaration of Helsinki, and was reviewed and approved by the Institutional Review Board of each center, including Hanyang University Seoul Hospital (HYUH IRB No. 2009-R-12). Written informed consent was obtained from all participants.
Data collection
Data were collected using a web-based electronic data capture system that included electronic case report forms from the Kor-ABP registry database. The following demographic and clinical characteristics were extracted: sex, age, body mass index (BMI), waist circumference (WC), extent of exercise, smoking status, alcohol intake, and traditional cardiovascular risk factors, including a history of hypertension, diabetes, dyslipidemia, stroke, myocardial infarction (MI), heart failure, and malignancy. Family history of hypertension, diabetes, and cardiovascular death was also obtained, along with data on antihypertensive drugs.
The following laboratory data were extracted: hemoglobin, triglyceride, total cholesterol, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol (LDL-C), estimated glomerular filtration rate (mL/min/1.73 m2), hemoglobin A1c, and fasting glucose. Left ventricular ejection fraction and left ventricular mass index (LVMI) were extracted from M-mode echocardiographic estimation data. Left ventricular hypertrophy (LVH) was defined as LVMI ≥ 116 g/m2 for men and ≥ 96 g/m2 for women.
ABPM data and definition of groups
A raw ABPM dataset was considered valid only if it contained at least 20 valid recordings from while awake and seven valid recordings from during sleep, after excluding unmeasured recordings and recordings with extreme BP (SBP ≥ 350 or < 60 mmHg; DBP ≥ 250 or < 30 mmHg) [
11]. Office BP was measured using a UA-767 monitor (A&D Co., Ltd., Tokyo, Japan), which had passed the European Hypertension Society protocol at all institutions. Office BP was determined as the mean BP of two measurements taken at 1 minute intervals with a 5-minute rest before the first measurement [
12].
MUCH was defined as the presence of 24-hour ambulatory mean SBP of ≥ 130 mmHg and/or DBP of ≥ 80 mmHg in patients treated with antihypertensive drugs with normal office BP (SBP of < 140 mmHg and/or DBP of < 90 mmHg), according to the international guideline criteria for MH [
1,
13]. Controlled hypertension was defined as 24-hour ambulatory mean SBP/DBP of < 130/80 mmHg and office SBP/DBP of < 140/90 mmHg in patients receiving an antihypertensive drug.
Statistical analyses
The study population with normal office BP was divided into two groups according to the presence of high 24-hour ABPM (controlled hypertension or MUCH). Continuous variables such as age, BMI, and WC, and categorical variables such as sex and number of antihypertensive drugs in the two groups were compared using Student’s t test and chi-square test, respectively. Fisher’s exact test was used for non-parametric analyses.
Because 8% of the data in the original dataset was missing (
Supplementary Fig. 1), we performed multiple imputations using a bootstrap expectation-maximization algorithm. Five possible imputed datasets were created, and the average value of the five imputed values was adopted as the missing values for the continuous variables. The most frequent value of the five imputed values was adopted for the categorical variables.
Univariate logistic regression analyses were used to evaluate the association between clinical factors and MUCH. To recognize the non-linearity of the associations with continuous variables (e.g., age, LVMI, heart rate [HR], BMI, and WC) and determine the optimal cut-off points for the variables, restrictive cubic spline fits were used in the univariate logistic regression analyses. A multivariate logistic regression model was developed to identify significant predictors of MUCH in patients with controlled office BP. All available potential confounders including age, sex, BMI, WC, exercise < 3 times/week, current alcohol intake or smoking, diabetes and dyslipidemia, history of stroke, MI or malignancy, family history of hypertension, diabetes or cardiovascular death, type and number of antihypertensive drugs, office SBP, office DBP, HR, and LDL-C levels were entered into the multivariate model as covariates to avoid prejudice. The multivariate model was reduced using a backward variable selection process to minimize overfitting of biases and to find the best-fit model (cut-off criteria, p < 0.05).
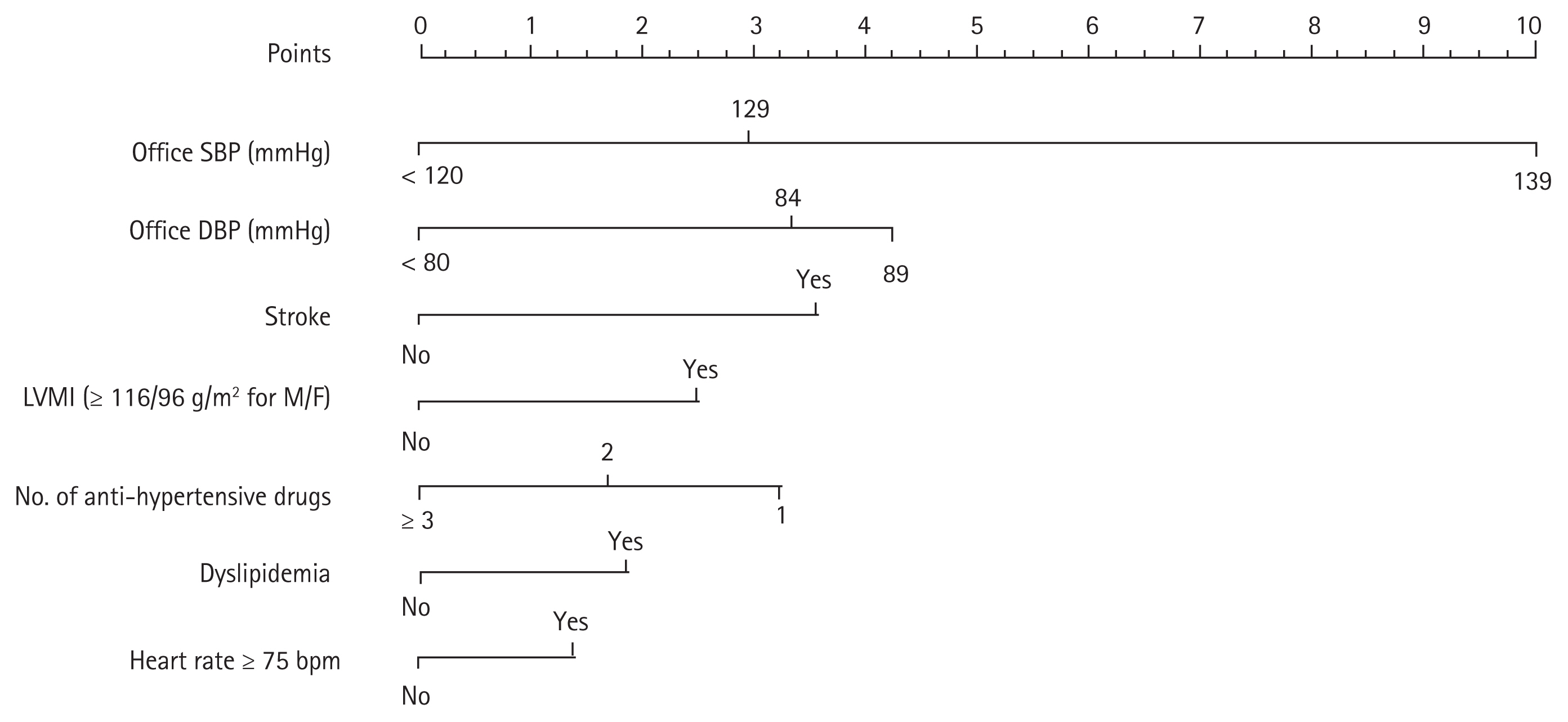
A prediction scoring system for MUCH was produced using the coefficients of significant predictors from the best-fit model. The largest among the coefficients of predictors was set as the integer 10, the maximum point in the nomogram, and the other coefficients were rescaled relative to the maximum point. The total score was calculated as the sum of the points assigned to all significant predictors included in the best-fit model, as previously described [
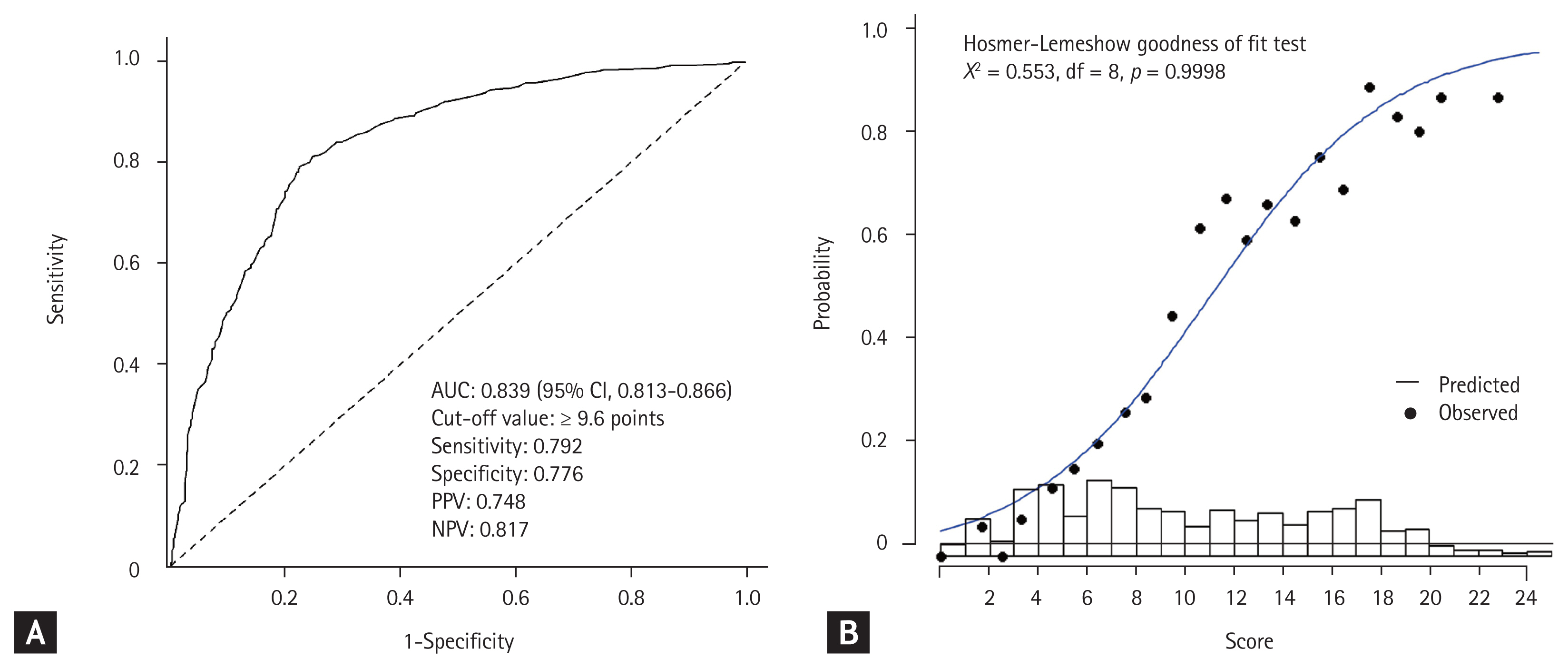
14]. Receiver operating characteristic (ROC) curve analysis was conducted using the linear predictors derived from the best-fit model to evaluate the performance of the prediction scoring system for MUCH. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated at an optimal cut-off point derived from Youden’s J-index. The goodness of fit between the predicted probability and the observed incidence of MUCH was evaluated using the Hosmer-Lemeshow test. The observed incidence of MUCH was calculated at every score interval of 1 for the Hosmer-Lemershow test.
We conducted internal validation and calibration of the best-fit model using bootstrap resampling [
15]. We validated the full logistic regression model with all covariates using 1,000 bootstrap resamples. In each bootstrap dataset, the full model with all covariates was reduced to a bootstrap model using a backward selection process, and optimism was estimated using the C-indexes of the best-fit and bootstrap models [
16]. The number of absolute errors between the predicted probability and the actual probability of MUCH in the best-fit model was also estimated through a calibration procedure using the same 1000 bootstrap re-samples.
All statistical analyses were performed using the statistical software R3.6.1, Rstudio1.2.1, and its packages including “descry,” “rms,” “Amelia,” “tableone,” “coin,” “ROCR,” and “pROC.” Statistical significance was set at p < 0.05.
DISCUSSION
In this study, we found that more than half of the patients on antihypertensive drugs who appeared to have controlled office BP actually had MUCH. Suboptimal office SBP and DBP levels, as well as underuse of antihypertensive drugs, increased HR, dyslipidemia, previous stroke, and LVH were strongly associated with an increased risk of MUCH. The proposed model employing these clinical predictors showed high accuracy for predicting the presence of MUCH in an outpatient clinic setting.
Guidelines for the management of hypertension [
13,
17,
18] emphasize the importance of 24-hour ABPM, making it important for the diagnosis of white-coat hypertension and MH. MUCH, which is defined by normal office BP and elevated out-of-office BP in patients receiving treatment for hypertension [
2,
9], can also be detected using 24-hour ABPM. Recent studies using meta-analyses, including prospective cohort studies, have shown that patients with MUCH face increased risks of cardiovascular events and all-cause death (hazard ratio, 1.80; 95% CI, 1.57 to 2.06) compared with patients with controlled hypertension [
9]. In addition, because of the high incidence of cardiovascular events and predictable cardiac events in MH [
19], it is important to know its clinical features and predictors in patients receiving hypertension treatment, especially in the MUCH subtype.
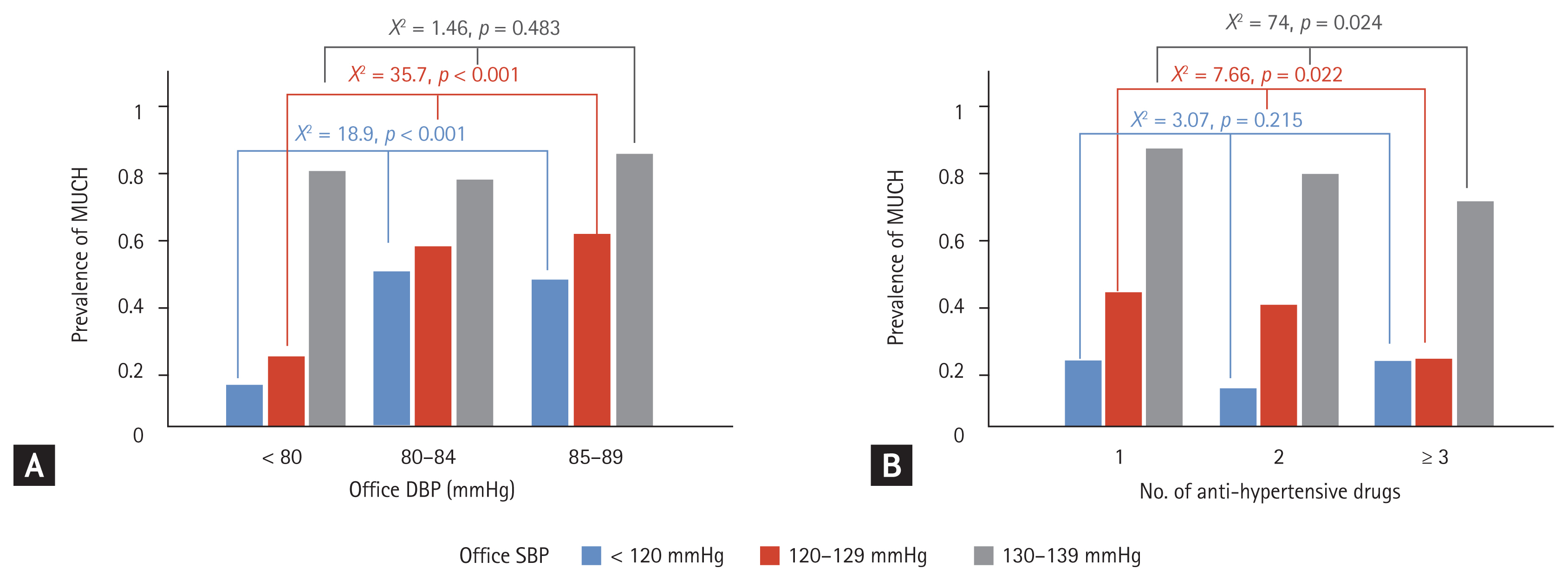
Our results underline the importance of the so-called high-normal office BP, which can be defined as an office SBP of 130 to 139 mmHg or DBP of 85 to 89 mmHg. The prevalence of MUCH increased 15-fold and 3-fold in patients with high-normal office SBP and DBP, respectively. A previous study using the Spanish Society of Hypertension ABPM registry data reported the prevalence of MUCH as 31.1% among patients with treated and controlled office BP (< 140/90 mmHg) [
1]. The researchers in the Spanish registry study showed that the presence of MUCH was also associated with high-normal office SBP and DBP, similar to our results.
Whether high-risk characteristics correlate with MUCH remains controversial. However, several studies have indicated that the risk profile of MH patients is in line with the risk profile of patients with MUCH. Metabolic disorders, including central obesity, hypertension, diabetes, and dyslipidemia, also increase the risk of MH [
20–
22]. Our results confirmed that patients with MUCH have more metabolic disturbances than patients with controlled hypertension. BMI ≥ 25 kg/m
2 and WC were significantly associated with MUCH, and dyslipidemia was an independent relevant factor for MUCH in our study. In addition, a history of stroke was an independent risk factor for MUCH. MH has been associated with a higher risk of stroke [
5], but the mechanism by which a history of stroke increases the risk of MH has yet to be determined. Moreover, one of the markers of target organ damage, LVH, was associated with MUCH in our study. Therefore, it seems reasonable to perform ABPM in individuals with these metabolically high-risk characteristics or target organ damage, such as LVH.
Previous studies have demonstrated that patients with excessive alcohol intake have an increased incidence of MH [
23,
24]. Ishikawa et al. [
23] reported that regular alcohol consumption increased the risk of MUCH by 1.76-fold in patients with stable hypertension. Our study supports previous findings that patients with MUCH were significantly more likely to be alcohol drinkers, with a 1.63-fold increased risk of MUCH compared to patients with controlled hypertension on univariate logistic regression analyses. Although current alcohol intake was not an independent risk factor for MUCH, in patients with high-normal BP or other metabolic risks, alcohol consumption may be considered and assessed as a factor affecting MUCH, regardless of the controlled-BP status.
In this study, we proposed a prediction model for MUCH that appeared to provide high diagnostic accuracy and goodness of fit for clinicians to identify patients with MUCH in outpatient settings using several easily available clinical features. The internal validation and calibration results obtained using the bootstrap resampling technique also showed sufficient reliability and validity of the model. It may be difficult for clinicians to notice the presence of MUCH in regular outpatients on antihypertensive drugs, since the condition is asymptomatic and, to date, office BP remains the main BP measurement tool and lacks any widely known clinical clues suggestive of MUCH. As MUCH is highly prevalent in patients with apparently controlled BP and is known to result in worse clinical outcomes [
9], clinicians should be mindful of identifying MUCH in those patients with the predictors for MUCH. Although sufficient external validations are required, the proposed prediction model may be useful in providing clinical cues for clinicians to prescribe ABPM in regular outpatients on antihypertensive drugs who satisfy some of the predictors.
Furthermore, the strong association between high-normal office BP and the lower number of antihypertensive drugs in the prediction model could provide the valuable insight that suboptimal office BP control through the underuse of antihypertensive drugs plays an important role in the development of MUCH. The significant interaction between the number of antihypertensive drugs and office SBP on the lower risk of MUCH may also underscore the role of suboptimal antihypertensive therapy in the development of MUCH. Although sub-analysis was performed according to the type of single antihypertensive drug used to evaluate whether the risk of MUCH varied with the drug of choice, there was no significant difference. Further study will be needed in the future to determine which combination of antihypertensive drugs affects the risk of MUCH. In addition to suboptimal office BP, studies to determine MUCH-specific parameters to filter out those patients with actual uncontrolled BP will be needed.
This study has several limitations. First, as with any cross-sectional study, the associations between the variables observed could not establish a causal relationship. Second, we did not assess medication non-compliance, a well-known cause of uncontrolled BP in patients on antihypertensive drugs. However, a recent study showed that unlike uncontrolled hypertension, MUCH is not attributable to medication non-adherence [
25]. Third, the duration of history of comorbidities, including hypertension and stroke, may be an important factor in uncontrolled hypertension, but data on these were insufficient. Approximately 8% of the original data were missing, with the rate of missing values varying from 0% to 58% among the variables. We did not exclude records with missing values and performed multiple imputations to prevent a loss of statistical power due to exclusion of data [
26]. Although multiple imputation using a bootstrap expectation-maximization algorithm is a frequently employed method for imputations, imputed data may have had unanticipated effects on the results. Finally, we validated and calibrated the prediction model internally using bootstrap resampling. Although resampling is a well-established method for internal validation, external validation using an independent dataset derived from a similar clinical settings will provide more confidence in the model.
MUCH is highly prevalent in patients with apparently controlled office BP. A borderline increase in office SBP and DBP, and underuse of antihypertensive drugs, as well as dyslipidemia, increased HRs, previous stroke, and LVH are independently associated with the presence of MUCH, which underscores the role of suboptimal treatment of hypertension in the development of MUCH. Clinicians should be mindful of the presence of MUCH in patients with these predictors, and the proposed prediction model may serve as a useful screening tool for MUCH to provide a clinical cue to prescribe 24-hour ABPM to patients.





 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Supplement 1
Supplement 1 Print
Print



