 |
 |
| Korean J Intern Med > Volume 35(4); 2020 > Article |
|
Abstract
Background/Aims
As the novel coronavirus (coronavirus disease 2019 [COVID-19]) outbreak progresses rapidly, staying home is recommended for suspected patients; however, the safety of this recommendation is uncertain. In Korea, non-hospital facilities called “living and treatment centers (LTCs)” have been established since 5 March 2020. The LTCs provided a unique opportunity to evaluate the safety of selection criteria for low-risk groups.
Methods
Between 5 March and 9 April 2020, patients with COVID-19 who met the following criteria were admitted to the LTC; alert, age below 65 years old, no underlying disease or well-controlled underlying disease, body temperature below 38.0°C, whether taking antipyretics or not, and no dyspnea. Patients were closely observed by doctors or nurses’ interviews twice a day and transferred to hospitals when symptoms worsened.
Results
A total of 113 patients were admitted to the LTC; 52.2% were female, with a median age of 25 years (interquartile range, 21.5 to 39.5). Of 113 patients, 54 (47.8%) were asymptomatic at diagnosis, and 15 (13.3%) had no symptoms until they were released from isolation. During the follow-up period, two (1.8%) patients were transferred to a hospital but did not progress to severe status during hospitalization.
In December 2019, a new strain of beta coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), that causes coronavirus disease 2019 (COVID-19), emerged in Wuhan, China [1]. Subsequently, the virus quickly spread worldwide, and the World Health Organization (WHO) declared COVID-19 a pandemic on 11 March 2020 [2]. The number of patients is increasing rapidly, stressing health care systems. Hospitals are reporting a shortage of critical equipment for COVID-19 patient care, including personal protective equipment for healthcare workers, owing to the surge in demand [3].
In response, healthcare authorities recommend staying home for seven days instead of visiting hospitals immediately when COVID-19 symptoms occur [4,5]. This recommendation relies on the fact that most COVID-19 patients have mild disease and can recover without medical care. In the early report from China, 81% of laboratory-confirmed cases had mild to moderate illness, including non-pneumonia and pneumonia cases [6]. However, Guan et al. [7] reported that 35.7% of patients classified as non-severe at the point of admission received oxygen therapy during hospitalization, and 2.4% were admitted to an intensive care unit. Therefore, recommendations for staying home in all suspected COVID-19 patients can be dangerous because some patients presenting with mild symptoms could worsen subsequently, requiring treatment.
Since the first imported COVID-19 case from Wuhan, China, was confirmed on 19 January 2020, the Korean Government has maintained a strong quarantine system of admitting all confirmed cases to biocontainment units of hospitals [8]. On 20 February 2020, a massive outbreak occurred among a religious group in the south of Korea, Daegu, and the isolation hospital beds became scarce [9]. To meet the sudden increase in medical and isolation needs, the non-hospital facilities called “living and treatment centers (LTCs)” were established in collaboration with the government and tertiary hospitals. LTCs provided a unique opportunity to conduct prospective studies on COVID-19 patients presenting with mild symptoms. Therefore, this study evaluated the safety of non-hospital settings for mild COVID-19 patients describing detailed clinical progression of relatively young patients presenting with mild symptoms.
This study was conducted in one LTC operated by Seoul National University Hospital (SNUH), a tertiary teaching hospital in Korea. The process of converting the accommodation and training facility into an LTC is described previously [10]. Patients were isolated in single rooms. To minimize contact with infectious patients, a video consultation care system was established, and patients were educated to check body temperature using a thermometer, pulse rate, and oxygen saturation by pulse oximetry, and describe their symptoms. The LTC was operated from 5 March to 8 April 2020. On 9 April 2020, all patients who needed further isolation were transferred to another LTC.
The Korean Centers for Disease Control and Prevention (KCDC) classified severity of COVID-19 into four categories, namely extremely severe, severe, mild, and asymptomatic. Of KCDC’s severity classification, only mild or asymptomatic patients with confirmed SARS-CoV-2 infection by real-time reverse transcriptase chain reaction (rRT-PCR) were admitted to the LTC. Detailed admission criteria were as follows: (1) alert, (2) age below 50 years old, (3) no underlying disease or well-controlled underlying disease, (4) body temperature below 38.0°C, whether taking antipyretics or not, and (5) no dyspnea. In response to the explosive outbreak in the city of Daegu and Gyeosangbuk-do in late February 2020, patients between 50 and 65 years old satisfying the remaining criteria were also admitted to the LTC from the beginning of the center operation. Patients were released from the LTC when their SARS-CoV-2 rRT-PCR tests results; two tests performed with a 24-hour interval were negative.
At admission, detailed interviews were conducted on exposure history, diagnosis date, and symptoms before admission. During the stay at the LTC, the patients checked their symptoms twice a day and submitted them using the questionnaire in the smartphone application. Doctors and nurses checked the patient’s report and monitored patients using a video-consultation system twice a day. Chest radiography and rRT-PCR of respiratory specimens were performed regularly.
The study was approved by the Institutional Review Boards of SNUH (IRB No. H-2003-163-1112). Informed consent was waived by the board.
From 5 March to 9 April 2020, 113 patients were admitted to the LTC operated by SNUH; 52.2% were female, with a median age of 25 years (interquartile range [IQR], 21.5 to 39.5) and 5.3% patients had underlying diseases, of which most common were hypertension (3.5%) and diabetes (0.9%) (Table 1).
Of 113 patients, 54 (47.8%) were asymptomatic at diagnosis, and 15 (13.3%) had no symptoms until they were released from isolation. The most common symptom during isolation was sputum (57.5%), followed by rhinorrhea (42.5%), cough (40.7%), headache (24.8%), sore throat (16.8%), chest discomfort/dyspnea (15.9%), and a febrile/chilling sensation (15.0%). Sputum lasted the longest (median duration 11 days; IQR, 4.5 to 18.5), while febrile sensation and myalgia improved the quickest (Table 2). No symptoms were severe enough to limit daily activities. Nine (8.0%) of 113 patients demonstrated pulmonary infiltrations on chest radiography upon admission. Of the remaining 104 patients, four patients developed pulmonary infiltrations during isolation.
During the follow-up period, two (1.8%) patients were transferred to a dedicated COVID-19 hospital. One patient had shown progression of pulmonary infiltration on serial chest radiography, and the other complained of dyspnea requiring oxygen supply (1 L/min via nasal cannula), which was assumed to be caused by a panic disorder (Fig. 1). Both patients did not progress to severe status during the hospitalization. As of 9 April 2020, 99 patients were released from the LTC after meeting the de-isolation criteria (Fig. 1). Time intervals between diagnosis and release from isolation were not different between patients with or without symptoms (25 days vs. 21 days, p = 0.150).
When comparing patient under 50 years old with patients between 50 and 65 years old, there was no significant difference in clinical course, such as the rate of transfer to hospital (1/95 vs. 1/18, p = 0.318) and isolation periods (23 days vs. 21 days, p = 0.946).
Our observation cohort consisted of COVID-19 patients under 65 years old, presenting with no symptom or mild symptoms. Few cases had concomitant underlying diseases that were associated with poor prognosis. Through daily close observation, several characteristics of asymptomatic or mildly symptomatic COVID-19 patients were determined. First, clinical progression rate to severe disease, which requires oxygen therapy, was meager (1.0/1,290 patient-days; 95% confidence interval, 0 to 13.3/1,000), indicating that close observation of cases under 65 years old presenting with mild symptoms may not be required, especially during a shortage of medical resources. Second, comprehensive monitoring confirmed that there were considerable asymptomatic infected patients that remained so until the release from isolation. Third, patients between 50 and 65 years old satisfying the criteria for mild status showed similar prognosis as those under 50 years old. It indicated that age criteria for mild could be raised from 50 to 65 years.
The WHO-China report, published on 29 February 2020, estimated that actual asymptomatic infections appear to be extremely rare because most of the cases that are asymptomatic on the date of identification go on to develop symptoms [11]. Several recent studies have documented asymptomatic COVID-19 patients [12-15]. However, whether reported asymptomatic cases have no symptoms at all remains unclear [16]. Upon thorough observation of 113 cases, 15 (13.2%) were completely asymptomatic. The viral shedding period of asymptomatic patients was similar to that of symptomatic patients, which suggests that even asymptomatic patients might spread the SARS-CoV-2 for a considerable period.
Several reports have described the clinical outcome of COVID-19 patients presenting with no symptoms [13,15]. Wang et al. [13] reported that 70.9% (39/55) of asymptomatic cases developed pneumonia, and 3.6% (2/55) progressed to severe status with hypoxia and were treated with a heated humidified high-flow nasal cannula for 5 days. The fact that a patient diagnosed as asymptomatic could progress to severe respiratory distress requiring high-flow nasal cannula may raise concerns that observing patients presenting with mild symptoms in non-hospital settings could be dangerous. In our cohort, radiological pneumonia occurred in 10.6%, and low-dose oxygen therapy was required in 0.9% of patients, which was due to a panic attack rather than hypoxia. The different outcome between the two studies might be due to differences in the demographic characteristics of the populations. Here, all patients were under 65 years old, and median age was significantly low (25 years old vs. 49 years old).
As COVID-19 spreads rapidly, the shortage of medical resources has become a severe problem in many countries [3]. To cope with this scarcity and prevent transmission, several COVID-19 guidelines recommended that mildly ill patients stay home because they can recover without medical care [4,5]. However, the clinical course of COVID-19 presenting with mild symptoms has not been investigated extensively and there have been concern about progression to severe disease while staying home with mild symptoms. Our data convincingly shows that recommendation of staying home could be a safe alternative to hospitalization for those patients who meet the clinical criteria for mild COVID-19 and were capable to monitor vital signs and symptom changes by themselves. Education and precaution should be taken on the patients to prevent household transmission during staying home.
1. Clinical progression rate to severe disease was negligible in coronavirus disease 2019 patients who met the following criteria at diagnosis: alert, age below 65 years old, no underlying disease or well-controlled underlying disease, body temperature below 38.0°C, whether taking antipyretics or not, and no dyspnea.
2. There were considerable asymptomatic infected patients that remained so until the release from isolation.
3. “Living treatment centers” could be a safe alternative considering shortage of hospital beds.
Acknowledgments
The authors appreciate the Ministry of Health and Welfare, the Korean Centers for Diseases Control and Prevention, the Local Government of Gyeosangbuk-do and Mungyeong-si for the administrative support and military, police, and fire officers who contributed to the stable operation of the facility.
Figure 1.
Clinical course and outcome of coronavirus disease 2019 patients observed at the living and treatment center (LTC) operated by Seoul National University Hospital between 5 March 2020 and 9 April 2020. aOn 9 April 2020, 12 patients were transferred to another LTC due to center closure. The median isolation period of patients at the time of transfer was 35 days.
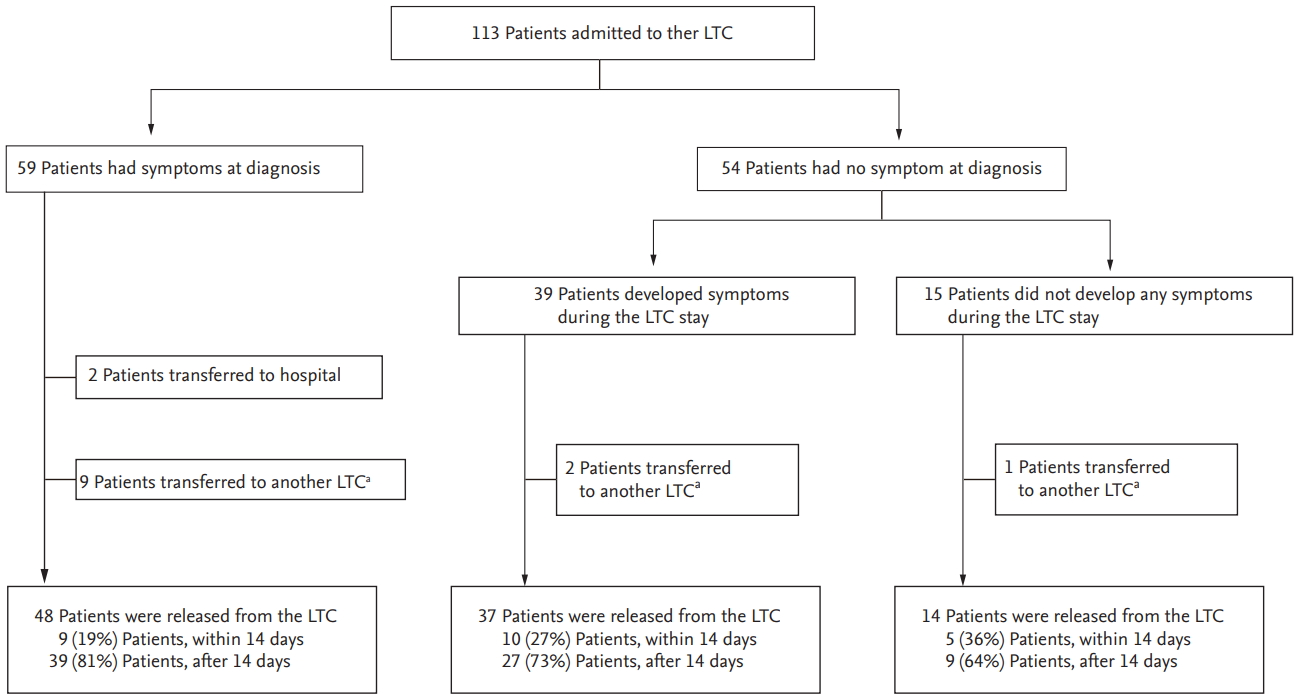
Table 1.
Demographic characteristics of coronavirus disease 2019 patients at the Living and Treatment Center according to presence of symptoms
| Characteristic | Total | Symptomatic at diagnosis | Asymptomatic at diagnosis and later symptomatic | Asymptomatic during the entire course |
|---|---|---|---|---|
| Total no. of patients | 113 | 59 | 39 | 15 |
| Male sex | 54 (47.8) | 32 (54.2) | 14 (35.9) | 8 (53.3) |
| Agea group | ||||
| 0–19 | 8 (7.1) | 3 (5.1) | 3 (7.7) | 2 (13.3) |
| 20–29 | 68 (60.2) | 34 (57.6) | 25 (64.1) | 9 (60.0) |
| 30–39 | 9 (8.0) | 8 (13.6) | 1 (2.6) | - |
| 40–49 | 10 (8.8) | 4 (6.8) | 3 (7.7) | 3 (20.0) |
| > 50 | 18 (15.9) | 10 (16.9) | 7 (17.9) | 1 (6.7) |
| Contact history with confirmed case | 43 (38.1) | 26 (44.1) | 13 (33.3) | 4 (26.7) |
| Underlying diseaseb | 6 (5.3) | 2 (3.4) | 3 (7.7) | 1 (6.7) |
| Smoking statusc | ||||
| Smoker | 4 (4.2) | 1 (2.0) | 3 (9.1) | 0 |
| Ex-smoker | 8 (8.3) | 6 (12.0) | 0 | 2 (15.4) |
| Non-smoker | 84 (87.5) | 43 (86.0) | 30 (90.9) | 11 (84.6) |
| Abnormal findings in chest radiography at admission | 12 (10.6) | 6 (10.2) | 4 (10.3) | 2 (13.3) |
| Isolation period, dayd | 23.0 (15.0–32.0) | 25.0 (17.0–33.5) | 21.0 (10.0–31.0) | 21.5 (8.3–31.3) |
Table 2.
Clinical feature of 113 coronavirus disease 2019 patients seen at the living and treatment center operated by Seoul National University Hospital between 5 March 2020 and 8 April 2020
REFERENCES
1. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in china, 2019. N Engl J Med 2020;382:727–733.



2. World Health Organization. WHO Director: general’s opening remarks at the media briefing on COVID-19: 11 March 2020 [Internet] Geneva (CH): WHO, c2020. [cited 2020 May 16]. Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020.
3. Ranney ML, Griffeth V, Jha AK. Critical supply shortages: the need for ventilators and personal protective equipment during the COVID-19 pandemic. N Engl J Med 2020;382:e41.


4. Centers for Disease Control and Prevention. What to do if you are sick [Internet] Atlanta (GA): CDC, c2020. [cited 2020 May 16]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/if-you-are-sick/steps-when-sick.html.
5. Public Health England. Stay at home: guidance for households with possible coronavirus (COVID-19) infection [Internet] London (UK): PHE, c2020. [cited 2020 May 16]. Available from: https://www.gov.uk/government/publications/covid-19-stay-at-home-guidance/stay-at-home-guidance-for-households-with-possible-coronavirus-covid-19-infection.
6. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020;323:1239–1242.


7. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020;382:1708–1720.


8. Kim JY, Choe PG, Oh Y, et al. The first case of 2019 novel coronavirus pneumonia imported into Korea from Wuhan, China: implication for infection prevention and control measures. J Korean Med Sci 2020;35:e61.



9. Korean Society of Infectious Diseases; Korean Society of Pediatric Infectious Diseases; Korean Society of Epidemiology; Korean Society for Antimicrobial Therapy; Korean Society for Healthcare-associated Infection Control and Prevention; Korea Centers for Disease Control and Prevention. Report on the epidemiological features of coronavirus disease 2019 (COVID-19) outbreak in the Republic of Korea from January 19 to March 2, 2020. J Korean Med Sci 2020;35:e112.




10. Lee SY, Kang EK, Kim YS, Cho BL, Kim MS, Jung HM. A suggestion from South Korea for treatment of mild or asymptomatic COVID-19 infected patients: living and treatment support center. Preprints 2020;2020040266. https://doi.org/10.20944/preprints202004.0266.v1.

11. World Health Organization. Report of the WHO-China joint mission on coronavirus disease 2019 (COVID-19) [Internet] Geneva (CH): WHO, c2020. [cited 2020 May 16]. Available from: https://www.who.int/publications-detail/report-of-the-who-china-joint-mission-on-coronavirusdisease-2019-(covid-19).
12. Rothe C, Schunk M, Sothmann P, et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med 2020;382:970–971.



13. Wang Y, Liu Y, Liu L, Wang X, Luo N, Li L. Clinical outcomes in 55 patients with severe acute respiratory syndrome coronavirus 2 who were asymptomatic at hospital admission in Shenzhen, China. J Infect Dis 2020;221:1770–1774.



14. Kimball A, Hatfield KM, Arons M, et al. Asymptomatic and presymptomatic SARS-CoV-2 infections in residents of a long-term care skilled nursing facility: King County, Washington, March 2020. MMWR Morb Mortal Wkly Rep 2020;69:377–381.



15. Zhou X, Li Y, Li T, Zhang W. Follow-up of asymptomatic patients with SARS-CoV-2 infection. Clin Microbiol Infect 2020;Mar. 28. [Epub]. https://doi.org/10.1016/j.cmi.2020.03.024.

16. Kupferschmidt K. Study claiming new coronavirus can be transmitted by people without symptoms was flawed [Science Magazine] [Internet] Washington (DC): American Association for the Advancement of Science, c2020. [cited 2020 May 16]. Available from: https://www.sciencemag.org/news/2020/02/paper-non-symptomatic-patient-transmitting-coronavirus-wrong.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



