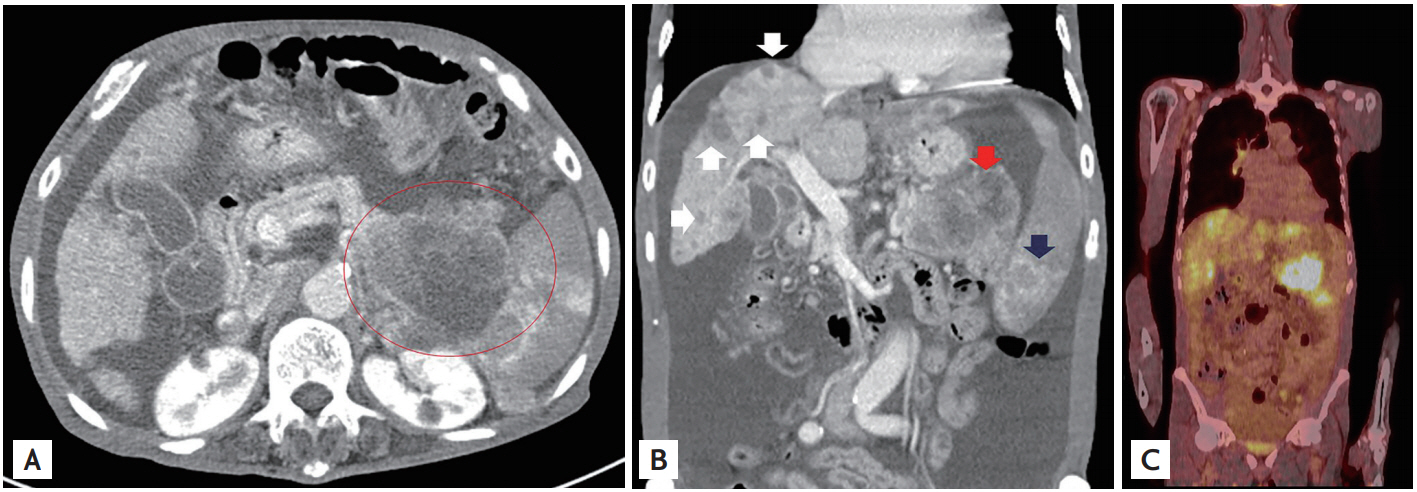
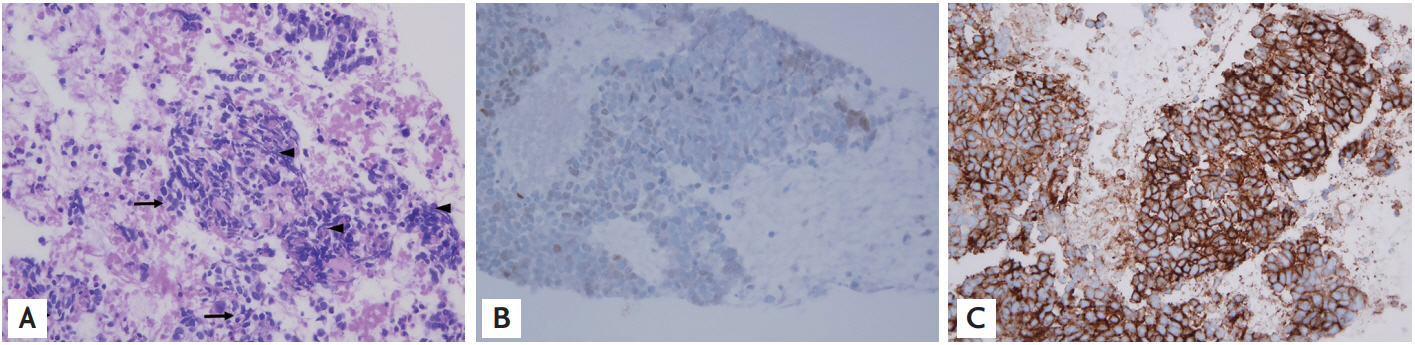
A 75-year-old man without underlying disease was referred to our department presenting with abdominal distension. Laboratory tests were unremarkable except for a significant elevation of carbohydrate antigen 19-9. An abdominal computed tomography (CT) scan demonstrated an approximately 8 cm-sized mass with a necrotic portion in the pancreatic tail and multiple hypodense masses involving liver, spleen, and adrenal gland with massive ascites (Fig. 1A and 1B). A chest CT scan showed no evidence of pulmonary tumor. A positron emission tomography scan revealed intense hypermetabolic uptake in the pancreatic tail, liver, spleen, both adrenal glands, and peritoneum (Fig. 1C). Endoscopic ultrasonography (EUS) showed an ill-defined heterogeneous mass in the pancreatic tail with peripancreatic and perihilar lymph node enlargement. EUS-guided fine needle biopsy (FNB) was performed with 22-G core needle on the pancreatic mass. On histology, small round cells with nuclear molding and crush artifacts (Fig. 2A). Immunohistochemical (IHC) staining was negative for thyroid transcription factor (TTF-1), leucocyte common antigen, and positive for CD56, which was compatible with primary pancreatic small cell carcinoma (PPSCC) (Fig. 2B and 2C). The patient refused palliative chemotherapy and expired 3 weeks later.
PPSCC is extremely rare, accounting for less than 1% of primary pancreatic malignancies. PPSCC has aggressive behavior and is usually diagnosed at an advanced stage. Therefore, the survival duration may be very short, although there are several reports of patients with PPSCC achieving partial or complete remission after combination chemotherapy. Cross-sectional imaging and IHC staining by EUS-FNB of obtained tissues are useful for determining whether a pancreatic small cell carcinoma is primary or metastatic. PPSCC diagnosis can be made in the absence of an abnormal pulmonary pathologic condition and is compatible with histopathologic results showing round to spindle-shaped small cells immunoreactive for CD56, chromogranin, and synaptophysin, but negative for TTF-1. Here, we report a rare case of PPSCC with poor prognosis and diagnosed by EUS-FNB using a 22-G core needle.
Written informed consent were obtained.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print





