INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is the fourth most common cause of the death in the United States and is projected to be the third most common cause of death by 2020 [
1]. COPD and cardiovascular disease are two of the leading causes of morbidity and mortality in the United States. Several studies have shown associations between COPD and angina, and COPD with angina increases hospital admission rate and mortality [
2]. Determining the clinical significance of angina as a comorbidity is important in patients with COPD because age distribution, risk factors, and clinical manifestations are similar under both conditions. Symptoms related to angina, such as chest discomfort, chest pain, and dyspnea on exertion, are also commonly reported symptoms in patients with COPD and their presentation could be misinterpreted as COPD symptoms [
3], and such patients with angina symptoms need cardiac evaluations. However, a noninvasive test can be problematic in these patients. Exercise tests, like treadmill tests, may not be performed due to ventilatory limitations in exercise and may not give satisfactory results. Pharmacological stress tests may be associated with bronchospasm [
4,
5]. Thus, coronary angiography (CAG) is the appropriate method for evaluating patients with COPD who also have angina symptoms. Many studies have examined angina and prognosis in patients with COPD. However, in those studies, the diagnoses of angina were made on clinical grounds or based on noninvasive tests rather than angiography [
6-
8].
The aim of this study was to evaluate the prognosis, including rates of hospitalization and death with significant coronary artery lesions and nonsignificant coronary artery lesions, in patients with COPD.
METHODS
Study population
We retrospectively reviewed medical records of 134 patients who had undergone CAG between January 2005 and December 2010 at Seoul National University Hospital, a tertiary referral hospital. All patients were ≥ 40 years of age, had smoking histories or were current smokers, and underwent pulmonary function tests. Patients with no history of smoking were excluded. Patients with a previous history of myocardial infarction, percutaneous coronary intervention (PCI), coronary artery bypass graft (CABG), lung cancer, or any other malignancy with lung metastasis, underlying interstitial lung disease, and pre-operation workup CAG were also excluded. In total, 113 patients were enrolled for analysis (
Fig. 1). Our study was approved by the institutional review board of Seoul National University Hospital.
Definitions and methods
COPD was defined according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines, with a post-bronchodilator forced expiratory volume in 1 sec/forced vital capacity (FEV1/FVC) ratio of < 70%. COPD severity was graded as mild (FEV1 > 80% predicted), moderate (FEV1, 50-80% predicted), severe (FEV1, 30-50% predicted), or very severe (FEV1 < 30% predicted). According to the GOLD, a clinical diagnosis of COPD should be considered in any patient who has dyspnea, chronic cough or sputum production, and/or a history of exposure to risk factors for the disease. The diagnosis should be confirmed by spirometry. Angina symptoms include retrosternal pressure, chest pain, or tightness worsened by exertion and relieved by rest or nitroglycerin. Sudden aggravation of dyspnea that could not be explained by COPD was also included in angina symptoms. All patients underwent an examination by a cardiologist at least once and were followed for at least 6 months as an outpatient.
CAG was performed after clinical evaluation by at least one specialized cardiologist. Significant coronary artery disease was defined as stenosis of more than 50% of the diameter at one or more major epicardial artery. The number of vessels with significant stenosis was counted and classified as 0-, 1-, 2-, or 3-vessel disease.
Major prognostic indicators included assessment of mortality and hospitalization rates. All-cause mortality and cause-specific mortality were investigated. In the case of death during hospitalization, the cause of death was analyzed from the death certificate written by the physician in charge and for patients who died outside of Seoul National University Hospital, it was analyzed by the death certificate from Statistics Korea. Causes of death were classified as respiratory-related death, cardiac death, sudden death, and other causes. Admissions due to cardiovascular, pulmonary, and cerebrovascular problems were included for analysis and other reasons, such as elective admission for CAG, were excluded. We analyzed clinical characteristics including age, gender, body weight, height, pulmonary function test, smoking history, follow-up duration, admission rate, intensive care unit (ICU) admission rate, and mortality rate, depending on the presence of a significant coronary artery lesion.
Statistical analysis
Quantitative variables are expressed as mean ± SD, and qualitative variables as numbers and percentages. Differences between independent groups were assessed by t tests for quantitative data and chi-square tests for qualitative variables. Mortality and admission rate depending on significant coronary lesion were analyzed by the Kaplan-Meier method. All statistical analyses were performed using the SPSS version 19.0 (SPSS Inc., Chicago, IL, USA). A two-tailed p value of < 0.05 was considered to indicate statistical significance.
RESULTS
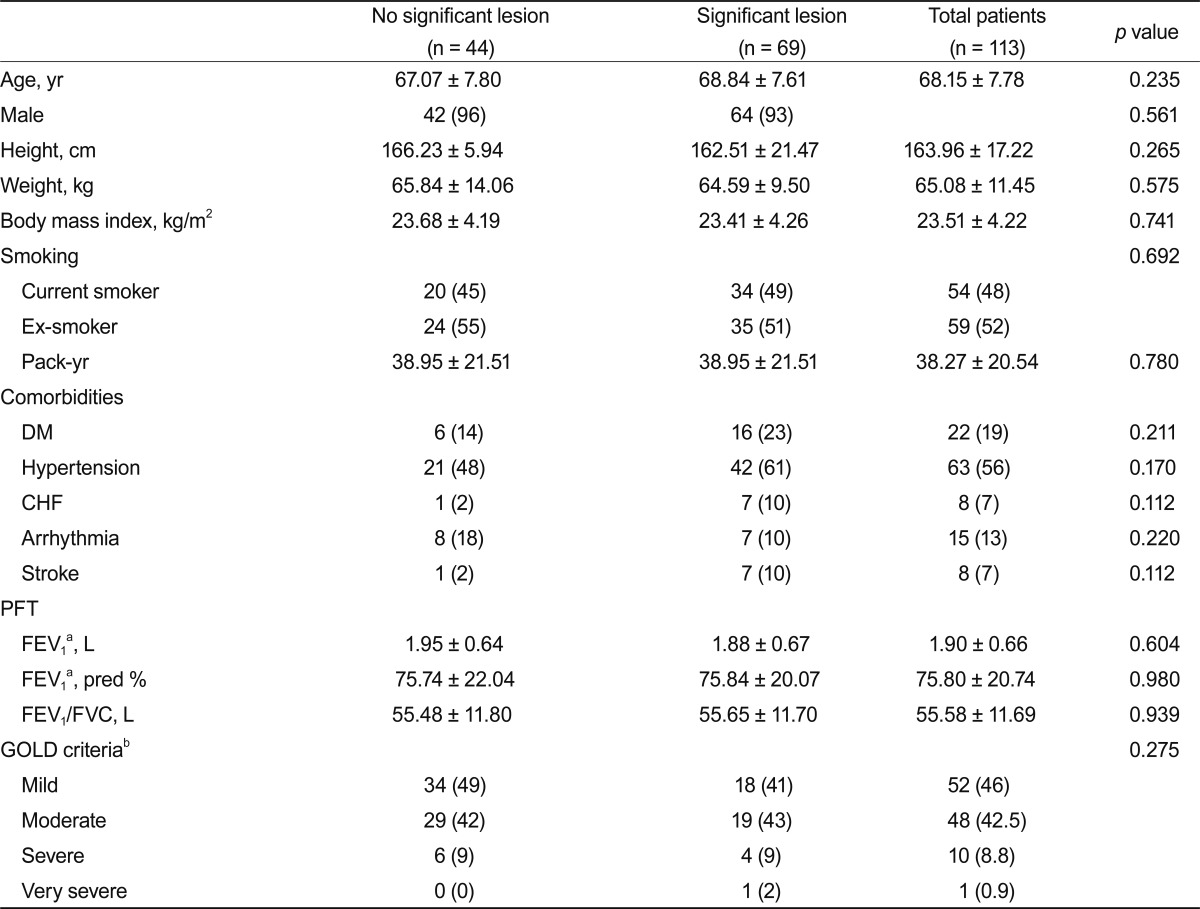
In total, 113 patients were enrolled: 106 (93%) were men and the mean age was 68.15 ± 7.80 years. Mean follow-up duration was 39 ± 21 months and the total amount of person-time was 588 person-years. Mean FEV
1 was 1.91 ± 0.66 L (predicted 75.8 ± 20.74%). Most of the patients had mild or moderate COPD (88%). Baseline demographic and clinical characteristics of patients with and without significant coronary lesions are summarized in
Table 1, showing that no significant difference existed between the two groups.
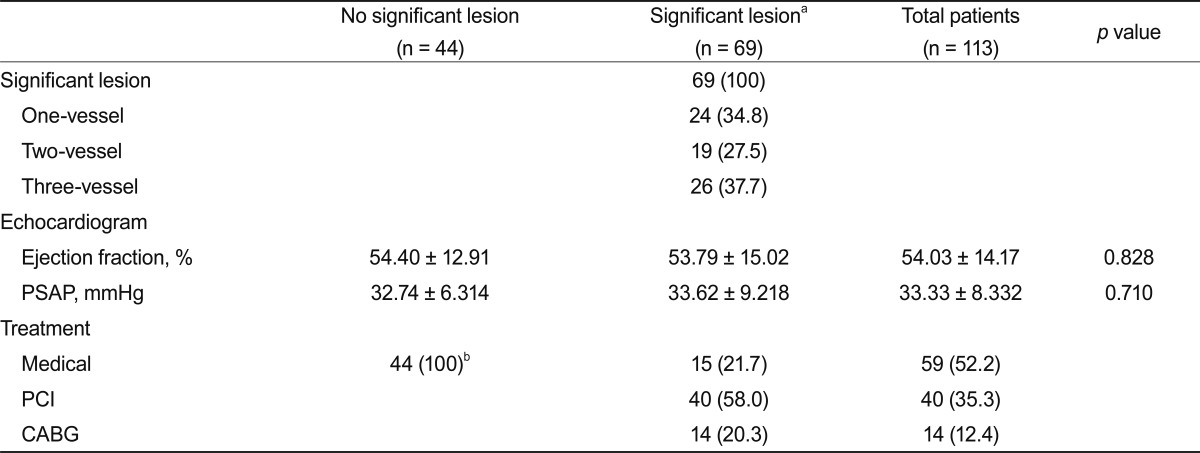
Of the patients with COPD, 69 (61%) had significant stenosis on CAG. Specifically, 24 patients (34.8%) had 1-vessel disease, 19 patients (27.5%) had 2-vessel disease, and 26 patients (37.7%) had 3-vessel disease. Among the patients with significant coronary lesions, 40 (58.0%) received PCI treatment, 14 (20.3%) underwent CABG and the other 15 patients (21.7%) received medical treatment. The patients without significant lesions received medical treatment only. Final diagnoses were chronic stable angina in 70 patients (62%), variant angina in 7 (6%), and stable angina in 18 (16%). In 18 patients (16%), we could not find a definitive cause of chest discomfort. No significant difference was detected in ejection fraction based on echocardiographic findings between the two groups. Pulmonary artery systolic pressure data were obtained from 58 patients and showed no difference between the groups (
Table 2).
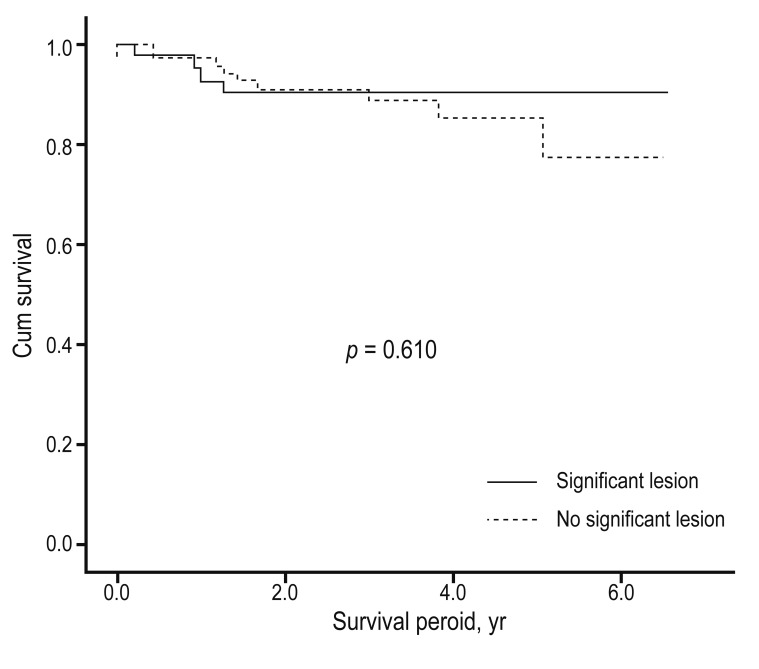
Thirteen patients (11.6%) died during the follow-up period. The rate of death during the follow-up period was 2.21 per 100 patient-years (3.98 per 100 patient-years in the group with angiographic significant lesions and 1.10 per 100 patient-years in the group without significant lesions). For cause-specific mortality, cause of death data could be obtained for only 11 patients; for the other two, we could not obtain cause of death data. Of the 11, four (36.3%) were respiratory-related deaths, five (45.4%) were cardiac-related deaths, one (9%) was cancer-related, and one (9%) was a case of sudden death. The causes of respiratory-related deaths were pneumonia in two patients, acute respiratory distress syndrome in one, and acute exacerbation of COPD (AECOPD) in one. The causes of cardiac death were congestive heart failure in three patients and acute coronary syndrome in two. Cardiac cause of death did not differ between the significant lesion and no significant lesion groups (
p = 0.160) (
Fig. 2). However, death due to acute coronary syndrome was seen only in the significant lesion group.
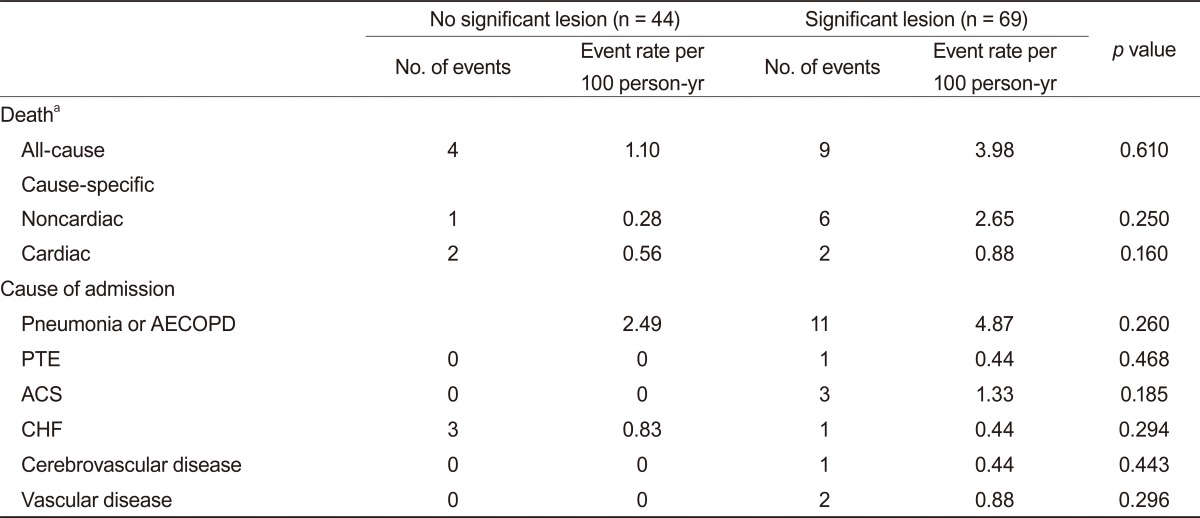
The admission rate was 10.17 per 100 patient-years in the group with significant lesions and 3.59 in the group without significant lesions. The ICU admission rates were 0.55 and 1.76 per 100 patient-years in patients with and without significant lesions. No significant differences were observed among the all-cause mortality rate, admission rate, or ICU admission rate in patients who had COPD with or without coronary artery disease (
Table 3).
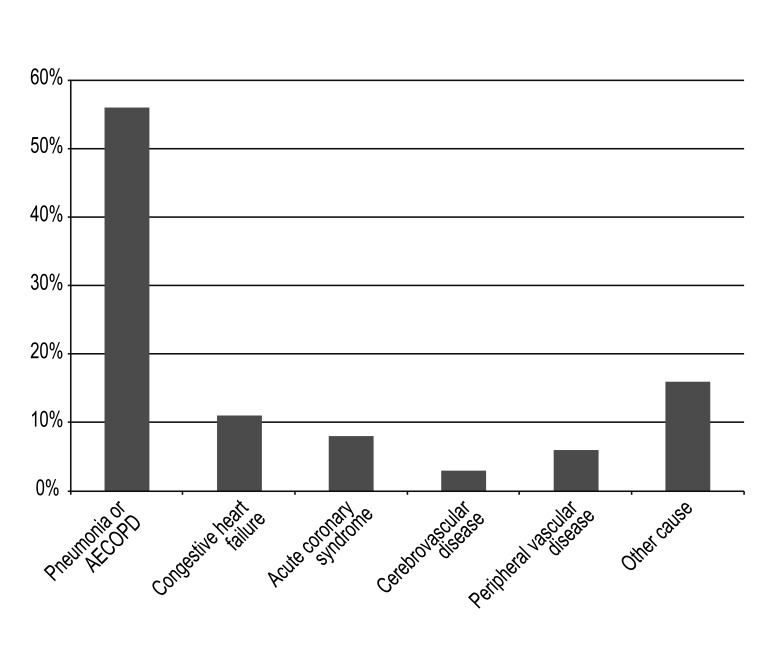
The total number of admitted patients was 18 (16%) and the total number of admissions was 36 cases. Pneumonia or AECOPD was most common cause of admission, occurring in 20 (56%) cases. Acute coronary syndrome occurred in three (8%) cases and congestive heart failure in four (11%) (
Fig. 3,
Table 4). Six (5%) patients were admitted to the ICU: all died during follow-up and four of them died in the hospital.
DISCUSSION
We studied 113 patients having COPD with angina who underwent CAG. In our study, significant coronary artery disease was detected in 61% of the total COPD patient population. In a small study, CAG was performed in 60 patients over 40 years of age and ischemic heart disease was diagnosed in 53.3% of them [
9]. Our study showed no statistically significant prognostic difference, including mortality and admission rate, in patients with COPD and angina depending on the presence of significant coronary artery lesions.
In patients undergoing CAG for suspicion of angina, the incidence of normal or near-normal coronary angiographic findings varied between 10% and 30%, depending on the characteristics of the patient group studied [
10]. Our study had a slightly higher incidence of normal or near-normal arteries and lower detection of significant lesions compared with other studies examining patients who had angina without COPD [
11]. We assume that it was due to the presence of endothelial dysfunction, which is associated with systemic inflammation and may explain angina with normal or near-normal coronary arteries. Patients with COPD have increased systemic inflammation. Thus, even if we found normal findings in CAG, some inflammation in those patients may still induce angina symptoms. Long-term cigarette smoking is also associated with impaired endothelium-dependent coronary vasodilation, regardless of the presence or absence of atherosclerotic wall thickening [
12]. Thus, these results are thought to be due to the high proportion of anatomically normal coronary angina.
Daly et al. [
11] demonstrated that the mortality rate of stable angina was 1.5 per 100 patient person-years. In the angiography-confirmed lesion group, the mortality rate was 1.8 per 100 patient person-years. Many studies have demonstrated that the coexistence of COPD and coronary artery disease leads to high morbidity or mortality [
6-
8,
13]. The mortality rate in our study was higher than that of prior studies in stable angina without COPD because of differing study populations. Patients with confirmed coronary lesions have a worse prognosis compared with those with no significant lesion [
11,
14]. Our study, however, showed no mortality or admission rate difference in the groups with and without significant lesions. One possible explanation for the lack of a difference in our study may be the relatively short follow-up period and small study population compared with other angina studies. In the Coronary Artery Surgery Study study, 12-year survival in 3,833 patients with stable angina was investigated and in the Duke Hospital Study, the 5-year survival rate of 2,842 stable angina patients was examined [
15,
16]. The follow-up period in our study was 2 years, shorter than in the other studies. In our study, we excluded high-risk patients who had acute myocardial infarction or previous myocardial infarction or intervention and most of the patients were those with stable angina. Additionally, as an important prognostic factor for cardiovascular disease, left ventricular systolic function in both groups was near-normal. The short follow-up and 2-year mortality may not adequately reflect the outcomes in patients with COPD and angina. Mortality rates for longer-term follow-up will be needed.
Questions may be raised about whether aggressive intervention may increase the survival rate in the significant stenosis group. Taken together, when these study findings were compared with the treatment effects of drug treatment, PCI, or CABG, no particular difference was detected in chronic stable angina [
17,
18]. The majority of our study patients had chronic angina and whether a procedure was performed may not have significantly affected the prognosis.
The most common causes of death were respiratory- and cardiac-related deaths. Cardiac death and coronary artery stenosis did not show a statistically significant association. According to other reports, the presence of coronary artery disease was associated with higher cardiac mortality, but not in our study [
19]. We believe the difference may be due to the small sample size.
The most common causes of admission during the follow-up period were pneumonia and AECOPD. Admission for a heart problem was the next most common cause. In a study of patients with COPD using National Hospital Discharge Survey data, the patients showed an increasing trend in hospitalization and mortality for pneumonia, congestive heart failure, and ischemic heart disease [
7]. These results suggest that the correction of risk factors is important in patients with COPD.
Limitations of this study include its retrospective nature and the small sample size. The patients groups were limited to patients having COPD with angina, so a risk of selection bias exists. Furthermore, lung cancer or other malignancies with lung metastases were excluded, but the lung cancer incidence was difficult to determine. Additionally, CAG itself can be a limitation. Because CAG is a two-dimensional assessment method, the extent of a lesion may not be an accurate assessment in patients with moderate or diffuse coronary artery stenosis, and evaluating functional status in coronary stenosis was difficult. Regarding admissions, we only analyzed cases of hospital admission in one tertiary referral educational hospital.
In conclusion, the detection rate of significant coronary lesion in patients having COPD with angina was 69 (61%) and it was slightly lower than that of the stable angina population without COPD. The mortality rate recorded in our study was higher than that of prior studies of stable angina without COPD. However, no outcome difference, including mortality, was detected according to the existence of significant coronary lesions during a 2-year follow-up period.








 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print


