 |
 |
| Korean J Intern Med > Volume 27(1); 2012 > Article |
|
Abstract
Background/Aims
This study elucidated the prognostic factors for neurocardiogenic syncope in males in their late teens and early twenties.
Methods
Tilt-table testing (TTT) was performed on 665 males (age range, 17 to 27 years) following the Italian protocol. The subjects were tilted head-up at a 70° angle on a table for 30 minutes during the passive phase. If the passive phase was negative, the subjects were given sublingual nitroglycerin and tilted to the same angle for 20 minutes during the drug-provocation phase. The subjects with positive results were followed without medication. We analyzed factors related to the recurrence rate of syncope.
Results
Of 305 subjects (45.8%) with positive results, 223 (age range, 18 to 26 years) were followed for 12 months. The frequency of previous syncopal episodes ≥ 4 (p = 0.001) and a positive result during the passive phase (p = 0.022) were significantly related to a high recurrence rate. A positive result during the early passive phase (≤ 12 minutes) was significantly related to a higher recurrence rate than was that during the late passive phase (> 12 minutes; p = 0.011).
Neurocardiogenic syncope is the most common cause of syncope in patients without underlying disease [1]. Neurocardiogenic syncope has a peak incidence in subjects in their late teens and early twenties [2]. Tilt-table testing (TTT) is used widely to diagnose neurocardiogenic syncope. The positive rate of TTT with or without a history of syncope ranges from 23.8 to 74% [3-6]. Many researchers have studied treatments of neurocardiogenic syncope including salt intake [7], physical maneuvers [8,9], beta-blockers [10,11], midodrine [12], fludrocortisones [13], paroxetine [14], and cardiac pacing [15]; however, the results are conflicting. In general, the prognosis of patients with neurocardiogenic syncope is benign, although some patients experience not only recurrent syncopal episodes but also serious head injuries despite treatment. Therefore, the identification of high-risk patients is important for treatment and follow-up. The frequency of previous syncopal episodes has been reported to be the most powerful predictor of recurrent neurocardiogenic syncope [16-21]. No other prognostic factors have been confirmed for males in their late teens and early twenties. Therefore, this study sought to identify prognostic factors for neurocardiogenic syncope in males in their late teens and early twenties.
Consecutive males with unexplained syncope seen between September 2006 and September 2008 were included. Subjects with underlying disease or abnormal electrocardiograms (ECGs) and those taking any medications were excluded. Abnormal ECGs included rhythms other than sinus rhythm, right- or left-axis deviation, left- or right-ventricular hypertrophy, Mobitz type 2 second-degree atrioventricular block, complete atrioventricular block, left bundle-branch block, and pathological Q-wave and abnormal ST-segment or T-wave changes.
TTT was performed according to the Italian protocol [22,23]. The subjects fasted for at least 3 hours before the test. The subjects were monitored throughout testing with 3-lead electrocardiography and automated blood pressure cuff measurements every 2 minutes. The TTT consisted of passive and drug-provocation phases. After a 5-minute rest in the supine position, the subjects were tilted head-up to a 70° angle on the table for 30 minutes during the passive phase. If the passive phase was negative, the subjects were given sublingual nitroglycerin (0.4 mg) and tilted to the same angle for another 20 minutes during the drug-provocation phase. The endpoint of the TTT was the induction of syncope with significant hypotension. Positive results were classified into the following three types [22,24]: type 1 (mixed) was defined as hypotension and heart rate 40-60/minutes; type 2 (cardioinhibitory) was defined as heart rate < 40/minutes or asystole for ≥ 3 seconds; and type 3 (vasodepressor) was defined as pure hypotension without bradycardia. Hypotension was defined as decreased blood pressure causing syncope or signs of poor tissue perfusion. The subjects with positive results were educated on the prevention of syncope, including the avoidance of predisposing factors, lying down at the onset of prodromal symptoms, fluid or salt intake, and physical maneuvers. No medications were prescribed for subjects with positive results. The subjects were followed in the outpatient clinic or by telephone on a regular basis for 12 months. All subjects provided informed consent.
We analyzed the frequency of previous syncope, the TTT phase that gave a positive result, the TTT duration until a positive result, the types of neurocardiogenic syncope, and the recurrence rate of syncope during the follow-up period. The results are expressed as the mean ± SD or median (interquartile range, IQR) for data that were not distributed normally. The Mann-Whitney U test and Kruskal-Wallis test were used for statistical analysis of data that were not distributed normally. Univariate and multivariate logistic regression analyses were used to identify variables associated with the recurrence of syncope during the follow-up period. A p value < 0.05 was considered significant. The data were analyzed with the SPSS version 12.0 (SPSS Inc., Chicago, IL, USA).
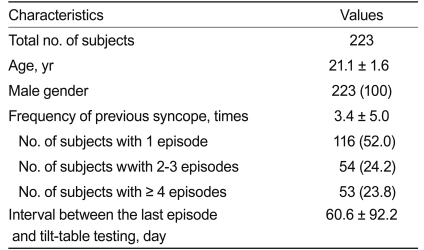
Of the 665 male subjects (mean age, 22.0 years; range, 17 to 27) who underwent testing, 305 (45.8%) had positive results on TTT. Of the subjects with positive results, 82 were excluded because of abnormal ECGs or loss to follow-up (Fig. 1). We followed 223 subjects (mean age, 21.1 years; range, 18 to 26) for 12 months. The frequency of previous syncopal episodes was 3.4 ± 5.0 (Table 1).
There were 45 (20.2%) subjects with positive results during the passive phase and 178 (79.8%) during the drug-provocation phase (Fig. 1). There were 146 (65.5%), 39 (17.5%), and 38 (17.0%) type 1 to 3 subjects, respectively. Syncope recurred in 67 (30.0%) subjects. The frequency of recurrence of syncopal episodes during the follow-up period was 1.3 ± 2.4. No recurrences occurred in 95 of 116 subjects (81.9%) with one previous syncopal episode, 36 of 54 subjects (66.7%) with two or three syncopal episodes, and 25 of 53 subjects (47.2%) with four or more syncopal episodes.
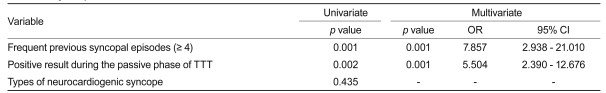
The subjects with four or more previous syncopal episodes in their lifetime had significantly more recurrences of syncopal episodes than did those with fewer than four (1, 2-3, and ≥ 4; 0 [IQR, 0 to 0.5], 0 [IQR, 0 to 2], and 3 [IQR, 0 to 9.5], respectively; p = 0.001) (Fig. 2). The subjects with positive results during the passive phase had significantly more recurrences of syncope than did those with positive results only during the drug-provocation phase (1 [IQR, 0 to 4] and 0 [IQR, 0 to 1], respectively; p = 0.022) (Fig. 3). The subjects (n = 7 of 45) with positive results during the early passive phase (≤ 12 minutes) had significantly more recurrences of syncopal episodes than did subjects (n = 38 of 45) with positive results during the late passive phase (> 12 minutes) (4 [IQR, 3 to 7] and 0 [IQR, 0 to 4], respectively; p = 0.011) (Fig. 3). However, there were no significant differences between the subjects with positive results during the early (≤ 10 minutes, n = 146 of 178) and late (> 10 minutes, n = 32 of 178) drug-provocation phases (0 [IQR, 0 to 2] and 0 [IQR, 0 to 0.5], respectively; p = 0.614) or among the types of neurocardiogenic syncope (types 1 to 3; 0 [IQR, 0 to 1], 0 [IQR, 0 to 3], and 0 [IQR, 0 to 3], respectively; p = 0.435) and the recurrence of syncope. Frequent previous syncopal episodes (≥ 4; p = 0.001) and positive results during the passive phase of TTT (p = 0.001) were significantly associated with the recurrence of syncope (Table 2).
This prospective, observational study elucidated prognostic factors for neurocardiogenic syncope in males in their late teens and early twenties in whom the incidence of neurocardiogenic syncope is high [2]. We found that most subjects (81.9%) with one previous syncopal episode had no recurrence and that frequent previous syncopal episodes in their lifetime (≥ 4), a positive result during the passive phase of TTT, and positive results during the early passive phase (≤ 12 minutes) were significantly related to the recurrence rate of syncope. Therefore, a positive result during the early passive phase of TTT and frequent previous syncopal episodes might be prognostic factors for neurocardiogenic syncope in males in their late teens and early twenties.
In previous studies, the frequency of syncope before TTT was the most powerful predictor for recurrent syncope [16-20]. Female gender, a history of bronchial asthma, and the number of previous syncopal episodes may predict recurrences of neurocardiogenic syncope [21]. However, the TTT phase or period associated with positive results as prognostic factors have not been studied in males in their late teens and early twenties.
Neurocardiogenic syncope occurs frequently during prolonged motionless standing, and the passive phase is similar to this situation. The drug-provocation phase is performed on subjects who can tolerate the passive phase. Such subjects were better able to tolerate prolonged motionless standing. Therefore, subjects with a positive result during the passive phase would tend toward a high recurrence rate of syncope. Furthermore, subjects with a positive result during the early passive phase could be more susceptible to a shorter duration of motionless standing.
The classification of neurocardiogenic syncope is based on the results of TTT [22,24]. The mechanisms of each type and the relationship between the type and prognosis are debatable [25].
For patients suspected of neurocardiogenic syncope, it is important to obtain a medical history and to perform TTT. Patients with positive results during the early passive phase of TTT and with more frequent episodes of previous syncope need to be followed closely and treated optimally.
The follow-up period of our subjects was relatively short; therefore, future prospective studies are needed to ascertain the recurrence of syncope in more subjects for longer periods of time at various centers. There are different TTT protocols (e.g., the Westminster protocol using isoproterenol for the drug-provocation phase). The Italian protocol with nitroglycerin is comparable to the Westminster protocol with isoproterenol [22,23].
References
1. Soteriades ES, Evans JC, Larson MG, et al. Incidence and prognosis of syncope. N Engl J Med 2002;347:878–885PMID : 12239256.


2. Colman N, Nahm K, Ganzeboom KS, et al. Epidemiology of reflex syncope. Clin Auton Res 2004;14(Suppl 1):9–17PMID : 15480937.

3. Youn HJ, Chung WS, Baek SH, et al. The usefulness of head-up tilt test in the diagnosis of syncope of unknown origin and clinical characteristics of the patients with vasovagal syncope. Korean J Med 1994;47:186–194.
4. Shinohara M, Kobayashi Y, Obara C, et al. Neurally mediated syncope and arrhythmias: a study of syncopal patients using the head-up tilt test. Jpn Circ J 1999;63:339–342PMID : 10943611.


5. Jeong JO, Kim JS, Kim JK, et al. Head-up tilt test in subjects with no history of syncope or presyncope. Korean Circ J 2000;30:841–846.

6. Turk U, Alioglu E, Kirilmaz B, et al. Prediction of head-up tilt test result: is it possible? Pacing Clin Electrophysiol 2010;33:153–158PMID : 19889180.


7. El-Sayed H, Hainsworth R. Salt supplement increases plasma volume and orthostatic tolerance in patients with unexplained syncope. Heart 1996;75:134–140PMID : 8673750.



8. Krediet CT, van Dijk N, Linzer M, van Lieshout JJ, Wieling W. Management of vasovagal syncope: controlling or aborting faints by leg crossing and muscle tensing. Circulation 2002;106:1684–1689PMID : 12270863.


9. Kim KH, Cho JG, Lee KO, et al. Usefulness of physical maneuvers for prevention of vasovagal syncope. Circ J 2005;69:1084–1088PMID : 16127191.


10. Sheldon R, Connolly S, Rose S, et al. Prevention of Syncope Trial (POST): a randomized, placebo-controlled study of metoprolol in the prevention of vasovagal syncope. Circulation 2006;113:1164–1170PMID : 16505178.


11. Nakagawa H, Kobayashi Y, Kikushima S, et al. Long-term effects of pharmacological therapy for vasovagal syncope on the basis of reproducibility during head-up tilt testing. Jpn Circ J 1998;62:727–732PMID : 9805252.


12. Kaufmann H, Saadia D, Voustianiouk A. Midodrine in neurally mediated syncope: a double-blind, randomized, crossover study. Ann Neurol 2002;52:342–345PMID : 12205647.


13. Scott WA, Pongiglione G, Bromberg BI, et al. Randomized comparison of atenolol and fludrocortisone acetate in the treatment of pediatric neurally mediated syncope. Am J Cardiol 1995;76:400–402PMID : 7639169.


14. Di Girolamo E, Di Iorio C, Sabatini P, Leonzio L, Barbone C, Barsotti A. Effects of paroxetine hydrochloride, a selective serotonin reuptake inhibitor, on refractory vasovagal syncope: a randomized, double-blind, placebo-controlled study. J Am Coll Cardiol 1999;33:1227–1230PMID : 10193720.


15. Connolly SJ, Sheldon R, Thorpe KE, et al. Pacemaker therapy for prevention of syncope in patients with recurrent severe vasovagal syncope: Second Vasovagal Pacemaker Study (VPS II): a randomized trial. JAMA 2003;289:2224–2229PMID : 12734133.


16. Sheldon R, Rose S, Flanagan P, Koshman ML, Killam S. Risk factors for syncope recurrence after a positive tilt-table test in patients with syncope. Circulation 1996;93:973–981PMID : 8598089.


17. Natale A, Geiger MJ, Maglio C, et al. Recurrence of neurocardiogenic syncope without pharmacologic interventions. Am J Cardiol 1996;77:1001–1003PMID : 8644623.


18. Grimm W, Degenhardt M, Hoffman J, Menz V, Wirths A, Maisch B. Syncope recurrence can better be predicted by history than by head-up tilt testing in untreated patients with suspected neurally mediated syncope. Eur Heart J 1997;18:1465–1469PMID : 9458453.


19. Kouakam C, Vaksmann G, Pachy E, Lacroix D, Rey C, Kacet S. Long-term follow-up of children and adolescents with syncope; predictor of syncope recurrence. Eur Heart J 2001;22:1618–1625PMID : 11492992.


20. Baron-Esquivias G, Errazquin F, Pedrote A, et al. Long-term outcome of patients with vasovagal syncope. Am Heart J 2004;147:883–889PMID : 15131546.


21. Aydin MA, Maas R, Mortensen K, et al. Predicting recurrence of vasovagal syncope: a simple risk score for the clinical routine. J Cardiovasc Electrophysiol 2009;20:416–421PMID : 19017338.


22. Sutton R, Bloomfield DM. Indications, methodology, and classification of results of tilt-table testing. Am J Cardiol 1999;84(8A):10Q–19Q.

23. Bartoletti A, Alboni P, Ammirati F, et al. 'The Italian Protocol': a simplified head-up tilt testing potentiated with oral nitroglycerin to assess patients with unexplained syncope. Europace 2000;2:339–342PMID : 11194602.


24. Brignole M, Menozzi C, Del Rosso A, et al. New classification of haemodynamics of vasovagal syncope: beyond the VASIS classification. Analysis of the pre-syncopal phase of the tilt test without and with nitroglycerin challenge. Vasovagal Syncope International Study. Europace 2000;2:66–76PMID : 11225598.


Figure 1
Flow diagram and number of subjects. Eighty-two patients were excluded because they were lost to follow-up or because they took medicine.
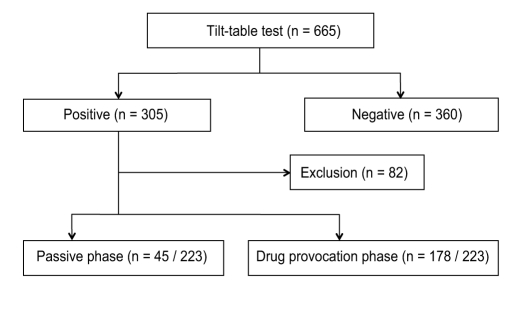
Figure 2
Recurrence of syncope according to the frequency of previous syncopal episodes. The results are expressed as the median (interquartile range).
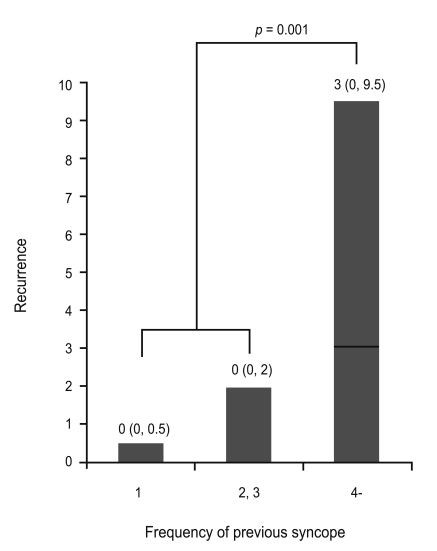
Figure 3
Recurrence of syncope according to the phase with positive tilt-table testing results. (A) Comparison of subjects with positive results during the passive and drug-provocation phases. (B) Comparison of subjects with positive results during the early and late passive phases. The results are expressed as the median (interquartile range).




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print



