INTRODUCTION
The incidence of colorectal cancer, the second leading cause of cancer-related death in Western countries, has been rising in developing countries, including Korea. Colorectal cancer is generally accepted to develop from an adenomatous polyp over several years [1,2]. Accordingly, the screening for precancerous adenomatous polyps and their subsequent endoscopic removal are known to prevent cancer development [3].
Ideal screening tests for colorectal cancer should be highly sensitive, as well as specific, safe, accepted by patients, and cost-effective [4,5]. Conventional colonoscopy (CC), the most commonly used screening test for colon diseases, not only shows high sensitivity and specificity in detecting precancerous polyps, but also allows for endoscopic polypectomy. However, because of discomfort and pain caused by CC, the majority of patients undergoing the procedure are given intravenous sedation, typically an opiate and a benzodiazepine, which in turn can lead to cardiovascular complications, including respiratory depression and hypotension [5-7].
Computed tomographic (CT) colonography, also referred to as virtual colonoscopy (VC), was first introduced in 1994 by Vining and colleagues [8]. This technique acquires data using helical or spiral CT scanning and generates high-quality two-and three-dimensional images of the colon lumen using specialized post-processing software. These images are then interpreted by a radiologist who can survey the colon lumen in any chosen direction [9]. VC, a noninvasive procedure, allows scanning of the entire large intestine in a short time and provides additional information on other organs. Furthermore, VC allows the examination of any anastomosis site, the colonic mucosa, the colonic wall, and other tissues surrounding the colon after surgical operations [10-14]. Until recently, the use of VC was limited to upper colon examinations for which CC is not available [15], although its use has gradually increased as a screening test for precancerous adenomas in adults without symptoms.
Although several studies have compared VC and CC in the diagnosis of precancerous polyps and colorectal cancers [12-14], most have not reported on patient acceptance and preferences for the two procedures. Patient acceptance and preferences are important factors for widely applicable screening tests, and cultural backgrounds may affect these factors with regard to VC and CC. Thus, we evaluated and compared patient acceptance and preferences for VC and CC in the diagnosis of precancerous polyps and colorectal cancers.
METHODS
Between August 2005 and July 2006, a prospective study was conducted involving 85 patients who visited the gastroenterology clinic for colorectal cancer screening or further evaluation of gastrointestinal (GI) symptoms, such as hematochezia, positive fecal occult blood test, iron-deficiency anemia, or personal/family history of colorectal neoplasia. In each, VC and CC were performed on the same day. All patients took a solution containing 90 mL of sodium phosphate and 120 mL of water for colon cleansing prior to the procedure. VC was performed first, followed by CC about 2-3 h later.
For VC, patients were asked to adopt a supine or prone position, and about 1,000-1,500 mL of air was injected through the anus before scanning, so as to inflate the whole colon. Then, with a spiral CT scan (HiSpeed Plus; GE Healthcare, Milwaukee, WI, USA), shots were taken every 0.7 mm from the diaphragm to the anus and three-dimesional images were reconstructed at the workstation.
CC was performed by an experienced endoscopist, with the patient under conscious sedation obtained by intravenous administration of midazolam 0.07 mg/kg and meperidine 50 mg. When sedation was incomplete, an additional 1 mg of midazolam was administered. After completing VC and CC, all patients were asked to complete questionnaires regarding abdominal pain, discomfort, and sense of dignity. A 7 point Likert scale was used, with the highest score representing the most unfavorable feeling [5]: 7, strongly dislike; 6, dislike; 5, somewhat dislike; 4, undecided; 3, somewhat like; 2, like; 1, strongly like. One questionnaire was conducted 2 h after CC when patients had recovered from the sedation. Patients were asked whether they had previously undergone CC or sigmoidoscopy, or had a barium enema. The quality of sedation during CC was assessed by patients as unsatisfactory, satisfactory, or good.
To evaluate the stability of the initial questionnaire answers after each procedure, a follow-up telephone questionnaire was conducted by a nurse within 24 h after the initial questionnaire. In the second questionnaire, questions about patient preferences for the screening tests were added.
For statistical analyses, the Wilcoxon signed-rank test was used to compare the degree of abdominal pain and discomfort, and the sense of dignity the patients felt during VC and CC. Spearman's rank correlation was used to compare symptoms immediately after the test and 24 h later.
Agreement between the questionnaires conducted immediately after each procedure and 24 h later was analyzed with kappa values. Using an ordinal scale, kappa values were converted to weighted kappa values, and kappa values 0<k<0.2 were interpreted as weak agreement, 0.2≤k<0.4 as moderate agreement, 0.4<k≤0.75 as strong agreement, and 0.75<k≤1 as very strong agreement [16]. Statistical analyses were performed using SPSS (version 12.0; SPSS, Inc., Chicago, IL, USA), and p values less than 0.05 were deemed to be statistically significant.
RESULTS
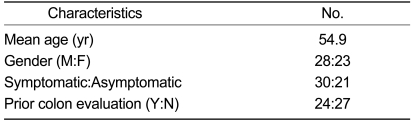
None of the patients experienced any serious complications after VC or CC. Among the 85 registered patients, 51 (28 men, 23 women) completed both the immediate and 24 h questionnaires. The mean age of the patients was 54.9 years old. Of the patients, 21 were referred for cancer screening and 30 for evaluation of GI symptoms. All patients reported that the quality of the sedation was satisfactory.
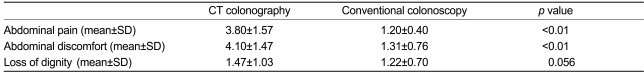
Of the 51 patients, 24 had previously undergone CC or sigmoidoscopy, or had a barium enema (Table 1). The mean scores for abdominal pain after the procedures were 3.80±1.57 (mean±SD) in VC and 1.20±0.40 in CC; the mean scores for abdominal discomfort were 4.10±1.47 in VC and 1.31±0.76 in CC, indicating more abdominal pain and discomfort in VC than in CC (p<0.01). A lower feeling of dignity was indicated by a score of 1.47±1.03 in VC and 1.22±0.70 in CC; VC showed a tendency for a worse score, but the difference was not significant (Table 2).
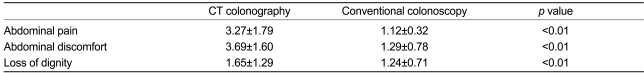
Table 3 summarizes the mean scores of symptoms 24 h after the procedure. The mean scores for abdominal pain were 3.27±1.79 in VC and 1.12±0.32 in CC; the mean scores for abdominal discomfort were 3.69±1.60 in VC and 1.29±0.78 in CC; the mean scores for a loss of dignity were 1.65±1.29 in VC and 1.24±0.71 in CC, indicating that abdominal pain and discomfort and loss of dignity were all worse in VC than in CC (p<0.01).
To examine the degree of agreement between the two questionnaires, a plot diagram was created for each symptom. The overall weighted kappa value ranged from 0.283 to 0.593, and thus the agreement between the two questionnaires was moderate-to-strong. Overall, 33 of 51 (64.7%) patients expressed a preference for CC, five (9.8%) preferred VC, and 13 had no preference. No differences were observed in terms of age, gender, existence of symptoms, or prior history of colon evaluations.
DISCUSSION
Regardless of age, gender, or presence of symptoms, patients in this study showed higher degrees of abdominal pain and discomfort and loss of dignity in VC versus CC. Accordingly, patients preferred CC to VC. According to Akerkar et al. [5], patients experienced more pain, discomfort, and loss of dignity in VC and would be willing to wait, on average, 4.9 weeks longer to receive CC rather than VC. This preference for CC may be partially explained by procedural circumstances. VC is performed with colon inflation while a conscious patient is in a relatively open space, causing more anxiety, loss of dignity, and discomfort. In contrast, CC is typically performed with the patients in a conscious sedated state, and the insertion of the endoscope and examination are performed by a doctor with a nurse in an isolated space, diminishing a patient's anxiety, loss of dignity, and discomfort.
The results of the present study differ from those of several previous reports, in which patients expressed a preference for VC [17-20]. In these studies, patients preferred VC because VC caused less abdominal pain or discomfort, which are closely associated with the quality of sedation. In the present study, all participants had satisfactory sedation during CC, and in our opinion, this influenced the patients' preference for CC.
Patient acceptance of VC and CC could vary depending on the patient's mental attitude before the procedure, which could be shaped by the information he or she had obtained and previous personal experiences [21,22]. A study reported that 50% of patients have a tendency to avoid the test because of their anxiety over CC [23]. Based on questionnaire results from 55 patients regarding VC and CC, Pineau et al. [10] reported that patients preferred VC before the procedure, but later expressed no preference. This finding suggests that although patient preference for CC was low before the procedure, due to anticipatory anxiety, it actually increased after the procedure [10]. In the present study, 24 (47%) of 51 patients had a history of prior colon evaluations, such as barium enema, CC, or sigmoidoscopy, but 27 patients (53%) underwent their first colon examinations. These two subgroups expressed no significant difference in abdominal pain or discomfort between VC and CC. However, the group with the history of colon evaluations indicated less loss of dignity 24 h after VC (p=0.01), although the two groups showed no significant difference in loss of dignity during CC. Thus, a prior history of colonic examination did not significantly affect patient acceptance in this study.
In terms of preferences, 33 (65%) of 51 patients expressed a preference for CC, five (10%) preferred VC, and the remaining 13 patients (25%) expressed no preference. In addition to less discomfort during the procedure, patients explained that they preferred CC because CC allowed for immediate biopsy and polypectomy, in addition to providing more accurate results. Patients who preferred VC reported that their decision was primarily due to the shorter procedure time of VC. Most of the patients who did not report a preference felt discomfort during bowel preparation, rather than during the procedure itself.
In the present study, we observed a difference in patient preference between VC and CC. This seemed to result in part from the use of sodium phosphate for bowel preparation, which caused less discomfort than polyethylene glycol. Sodium phosphate, however, has been reported to disturb serum electrolyte profiles, and thus its use is not recommended in patients suffering from congestive heart failure or chronic renal failure. To improve patient compliance with VC and CC for colorectal cancer screening, the development of alternative safe and comfortable bowel preparation methods is desirable [24].
In conclusion, the patients in this study showed acceptance of both types of colonoscopy, but they experienced more abdominal pain and discomfort and loss of dignity during VC than CC, and expressed a preference for CC over VC. Although VC is a safe and noninvasive screening test of colorectal cancer, further study is required to increase patient acceptance before replacing CC with VC.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print





