 |
 |
| Korean J Intern Med > Volume 22(3); 2007 > Article |
|
Abstract
Background
The role of Helicobacter pylori (H. pylori) in the pathogenesis of coronary artery disease (CAD) is still controversial, and the relation between current H. pylori infection and CAD has not been fully examined. This study evaluated the relation between H. pylori infection as confirmed by gastroduodenoscopic biopsy and CAD.
Methods
We determined the presence of H. pylori infections, via gastroduodenoscopy, in 88 patients of the normal coronary angiographic group and also in 175 patients of the CAD group, and the latter patients had more than 50% coronary stenosis angiographically demonstrated. We excluded those patients with a history of previous H. pylori eradication and/or malignancy. A small piece of tissue from the antrum, which was obtained by gastroduodenoscopic biopsy, was stained by Warthin-starry silver stain. We defined a negative staining result that there was no stained tissue in the sample and the stained tissue was also positive for H. pylori infection.
Results
There was no significant difference, except for gender, age, smoking and high density lipoprotein cholesterol (HDL-c), of the demographic and laboratory characteristics between the groups. Twenty seven (30.7%) patients of the normal control group and 71 (40.6%) patients of the CAD group were positive of H. pylori infection, yet there was no statistical difference. We angiographically followed up the 80 patients of the CAD group who were treated by percutaneous coronary intervention (PCI) at 6 to 9 months after their primary intervention. Twenty two (37.9%) of the 58 patients of the H. pylori negative group and 10 (45.5%) of the 22 patients of the H. pylori positive group were treated with reintervention, but reintervention was also not significantly different between the group with H. pylori infection and the group without the infection.
Helicobacter pylori (H. pylori) infection is an etiological factor for the development of peptic ulcer and gastric cancer1). Several preliminary reports have suggested that chronic infections by H. pylori, as well as other chronic infections, may be associated with atherosclerosis and vascular disease2, 3). However, most prospective studies have not confirmed the association between chronic infections and coronary artery disease (CAD)4-6) and all the recent prospective studies and meta-analyses on the association between Chlamydia pneumoniae (C. pneumoniae) and/or Cytomegalovirus infection and coronary disease have produced negative results. This suggests there is only a possible mild association, and the previous studies virtually excluded a major role for H. pylori infection as a risk factor7, 8). Several studies have assessed the association between the cytotoxin-associated gene-A (CagA) status and vascular diseases (either coronary disease or cerebrovascular disease), and these studies have produced mixed results9-13). The rate of positivity for H. pylori infection among Korean adults is reported to reach as much as 70%14-16). Though the prevalence of coronary artery disease among Asians has been reported to not be much different from that of Caucasians, in spite of the high rate of H. pylori infection for both races17), the exact relation between H. pylori and cardiovascular risk factors might be an important issue to reduce the incidence of cardiovascular disease18).
The objectives of the present study were to reveal and examine the relation between the H. pylori infection of the stomach and CAD, and to angiographically determine, after 6 to 9 months, the influence of H. pylori infection on the reintervention of patients who were treated by percutaneous coronary intervention (PCI).
The subjects of this study were those patients who were admitted to the Cardiac Catheterization Laboratory at Daejeon St. Mary's Hospital and Kangnam St. Mary's Hospital for coronary angiography, and these patients were suspected to have developed CAD; we prospectively enrolled those patients who were seen from January 2003 to June 2006. All the patients underwent physical examinations. In terms of smoking behavior, the patients were divided into two groups: smokers and non-smokers. Patients who had stopped smoking for 10 years or less were classified as smokers. The definition of hypertension was the current use of antihypertensive drugs, or it was based on the seventh report of the Joint National Committee on the Detection, Evaluation and Treatment of High Blood Pressure. Hyperlipidemia was defined as the state where the serum cholesterol level was 200 mg/dL and greater, or the current use of a hypolipidemic drug. The definition of diabetes was based on the criteria of the American Diabetes Association, or the current use of oral hypoglycemic agents or insulin. The decision to perform coronary angiography was based on those symptoms that were consistent with this diagnosis and also an abnormal electrocardiogram (either baseline or stress). Both the right and left coronary arteries were studied in at least two oblique projections (RAO 30┬░ and LAO 60┬░). The CAD group that was included in the study consisted of those patients who had at least one coronary artery lesion that occupied at least 50% of the luminal diameter, as noted on the coronary angiography. The patients who had normal coronary angiographic results were selected as the normal control group. Gastroduodenoscopy was done in both groups within 1 month before or after performance of the coronary angiogram. Some patients were excluded if they had a platelet count of less than 100,000/mm3, acute myocardial infarction within the 48 hours, primary PCI, a history of previous treated PCI or coronary artery bypass graft or H. pylori eradication or malignancy. A small tiny tissue of the antrum that was taken by gastroduodenoscopic biopsy was stained via Warthin-starry silver stain. A negative staining result was defined as there was no stained tissue in the sample and the stained tissue was positive for H. pylori infection. More than 70% of the coronary stenotic patients in the CAD group were angiographically treated with PCI. Procedural success was defined as the final diameter of the stenosis was 35% or less and there was no flow-limiting dissection. Intracoronary stents were recommended only for those patients with suboptimal angiographic results. We angiographically followed up, at between 6 to 9 months, the patients of the CAD group who were treated by PCI and we then we evaluated their reintervention; their new stonotic lesions were due to new coronary stenotic lesion and in-stent restenosis. New coronary stenotic lesion was defined when the newly developed lumen occupied more than 50% of the vessel lumen, and in-stent restenosis was defined when the blockage was more than 50% of the stent lumen. The height and weight of each patient was measured and the body mass index (BMI) was calculated as kg/m. After more than 12 hours of fasting, a blood sample was taken before the coronary angiogram. The blood glucose level, total cholesterol, triglyceride (TG), high-density lipoprotein cholesterol (HDL-c) and low-density lipoprotein cholesterol (LDL-c) and so on were measured by an enzymatic method and using an automatic analyzer (Hitachi 747). Highly sensitive C-reactive protein (hsCRP) was measured by immunonephelometry (Nephelometry, Behring Nephelometer II, Dade Behring Marburg, Germany).
Statistical analyses were performed with using SPSS11 statistical analysis software. Unless otherwise noted, any test of a hypothesis was two-sided and the level of significance was set at 5%. Potential associations between the clinical and biologic parameters were tested for by univariate analysis with using the Student t or the chi-square test. The results were expressed as means┬▒SDs.
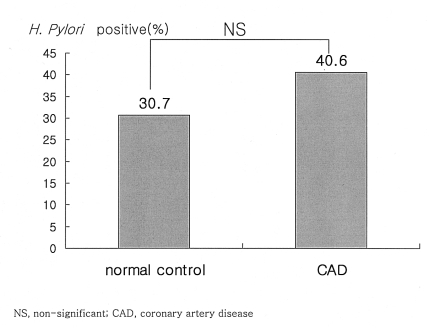
The series originally consisted of 88 cases for the angiographically documented normal control group and 175 angiographically documented cases for the CAD group. Compared with the normal control group, the patients with CAD were significantly older and smoked more and among them, the male patients outnumbered their female counterparts; in addition, the male CAD patients had lower serum concentrations of HDL-c (Table 1). Twenty seven (30.7%) patients of the normal control group and 71 (40.6%) patients of the CAD group were positive for H. pylori infection. The incidence of H. pylori infection for the CAD group showed a tendency to increase, but there was no statistical difference between the groups (Figure 1).
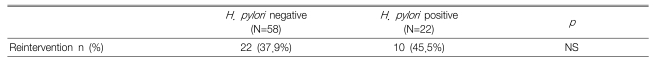
We angiographically followed up the 80 patients of the CAD group who were treated by PCI after 6 to 9 months (the re-intervention group). Twenty two (37.9%) of the 58 H. pylori negative patients and 10 (45.5%) of the 22 H. pylori positive patients were treated with reintervention, and the rate of reintervention was also not significantly different between the two groups (Table 2). The reintervention was caused by new coronary stenotic lesion and in-stent restenosis. New coronary stenotic lesions were noted in 18 (31.0%) of the 58 H. pylori negative patients and in 10 (45.5%) of the 22 H. pylori positive patients, and the number of patients with in-stent restenosis were 8 (13.8%) and 2 (9.1%), respectively. The previous stents of the in-stent restenosis patients were all bare-metal stents. There was no significant difference between the group with H. pylori infection and the group without the infection.
Seroepidemiologic studies have demonstrated that atherosclerosis is associated with several infectious pathogens, including H. pylori2, 19), C. pneumoniae20, 21) and cytomegalovirus22). Both H. pylori infection and CAD are associated with the socioeconomic status of patients, and both H. pylori infection and CAD increase with age23, 24). Finding a causal association between the two diseases would be very important in that H. pylori can be screened for and it is amenable to treatment. There is also the possibility of a future vaccine that might be given in childhood and also performing eradication of H. pylori in adulthood. Previous studies that examined the relation of both diseases have used a variety of criteria to define the presence or absence of CAD. In addition, all of the control subjects in the other previous studies have lacked angiographic confirmation2,25-27). Therefore, to minimize any misclassification of our patients, we used angiographic confirmation to determine the presence or absence of CAD in both the cases and the controls. In the other studies, the presence or absence of H. pylori seropositivity was used to diagnose H. pylori infection, yet in our study, this was diagnosed by gastroduodenoscopic biopsy1, 2, 4, 6, 7).
The results of our studies revealed little association between H. pylori infection and CAD, but the rate of H. pylori infection for the CAD group showed a tendency to increase. According to a recent study, chronic infection with H. pylori may be involved in the development of atherosclerosis via endothelial dysfunction and systemic and vascular inflammation28), and definite evidence of an association between CagA-positive H. pylori and ischemic heart disease will probably come about only from prospective studies. We found three group case-control studies4, 12, 13) that had remarkably similar results; these studies showed the weak association between CagA-positive H. pylori and the occurrence of fatal and nonfatal myocardial infarction during the follow-up period, with a pooled odds ration (OR) of 1.26 (95% confidence interval: 1.05-1.51), which corresponds to a relative risk of 1.13. These findings virtually rule out any major relationship between the CagA status and ischemic heart disease. A possible limit of these studies is that they were performed in the same country with a population that had a relatively high prevalence of CagA strains. However, the reported 13% increase in the risk of cardiac events may still have significant epidemiological consequences, as infection by CagA-positive H. pylori is present in approximately 30% of the population. In addition, H. pylori may be an independent risk factor for restenosis, and other studies have reported that H. pylori eradication significantly attenuates the reduction in the coronary artery lumen in CAD patients after PCI29, 30). In our study, the relation between H. pylori and reintervention after PCI also had a tendency to increase, but there was no significant difference.
There are several limitations in our study. The study included a small number of patients and we lacked information about the virulence of H. pylori. The number and rate of the followed-up patients that underwent reintervention were also small. We believe that future studies that will focus on the virulent H. pylori strains in a large group of patients are needed to determine the probable role of H. pylori for CAD and restenosis.
References
1. Huang JQ, Zheng GF, Sumanac K, Irvine EJ, Hunt RH. Meta-analysis of the relationship between CagA seropositivity and gastric cancer. Gastroenterology 2003. 125:1636ŌĆō1644PMID : 14724815.


2. Mendall MA, Goggin PM, Molineaux N, Levy J, Toosy T, Strachan D, Camm AJ, Northfield TC. Relation of Helicobacter pylori infection and coronary heart disease. Br Heart J 1994. 71:437ŌĆō439PMID : 8011406.



3. Danesh J, Collins R, Peto R. Chronic infections and coronary heart disease: is there a link? Lancet 1997. 350:430ŌĆō436PMID : 9259669.


4. Whincup PH, Mendall MA, Perry IJ, Strachan DP, Walker M. Prospective relations between Helicobacter pylori infection, coronary heart disease and stroke in middle aged men. Heart 1996. 75:568ŌĆō572PMID : 8697158.



5. Wald NJ, Law MR, Morris JK, Bagnall AM. Helicobacter pylori infection and mortality from ischemic heart disease: negative results from a large prospective study. BMJ 1997. 315:1199ŌĆō1201PMID : 9393222.



6. Folsom AM, Nieto JF, Sorlie P, Chambless LE, Graham DY. Helicobacter pylori seropositivity and coronary heart disease incidence. Circulation 1998. 98:845ŌĆō850PMID : 9738638.


7. Haider AW, Wilson PW, Larson MG, Evans JC, Michelson EL, Wolf PA, O'Donnell CJ, Levy D. The association of seropositivity to Helicobacter pylori, Chlamydia pneumoniae and cytomegalovirus with risk of cardiovascular disease: a prospective study. J Am Coll Cardiol 2002. 40:1408ŌĆō1413PMID : 12392829.


8. Ridker PM, Hennekens CH, Buring JE, Kundsin R, Shih J. Baseline IgG antibody titres to Chlamydia pneumoniae, Helicobacter pylori, herpes simplex virus and cytomegalovirus and the risk for cardiovascular disease in women. Ann Intern Med 1999. 131:573ŌĆō577PMID : 10523217.


9. Pasceri V, Cammarota G, Patti G, Cuoco L, Gasbarrini A, Grillo RL, Fedeli G, Gasbarrini G, Maseri A. Association of virulent Helicobacter pylori strains with ischemic heart disease. Circulation 1998. 97:1675ŌĆō1679PMID : 9591760.


10. Pasceri V, Patti G, Cammarota G, Pristipino C, Richichi G, Di Sciascio G. Virulent strains of Helicobacter pylori and vascular disease: a meta analysis. Am Heart J 2006. 151:1215ŌĆō1222PMID : 16781222.


11. Whincup P, Danesh J, Walker M, Lennon L, Thomson A, Appleby P, Hawkey C, Atherton J. Prospective study of potentially virulent strains of Helicobacter pylori and coronary heart disease in middle-aged men. Circulation 2000. 101:1647ŌĆō1652PMID : 10758045.


12. Stone AFM, Risley P, Markus HS, Butland BK, Strachan DP, Elwood PC, Mendall MA. Ischaemic heart disease and CagA strains of Helicobacter pylori in the Caerphilly Heart Disease Study. Heart 2001. 86:506ŌĆō509PMID : 11602541.



13. Singh RK, McMahon AD, Patel H, Packard CJ, Rathbone BJ, Samani NJ. Prospective analysis of the association of infection with CagA bearing strains of Helicobacter pylori and coronary heart disease. Heart 2002. 88:43ŌĆō46PMID : 12067941.



14. Malaty HM, Kim JG, Kim SD, Graham DY. Prevalence of Helicobacter pylori infection in Korean children: inverse relation to socioeconomic status despite a uniformly high prevalence in adults. Am J Epidemiol 1996. 143:257ŌĆō262PMID : 8561159.


15. Yong DG, Lee HM, Kim HS, Lee JG, Lee YC. Clinical usefulness of Helicobacter pylori IgG Ab assay: comparison of six commercial kits. Korean J Clin Pathol 1998. 18:447ŌĆō451.
16. Kim KH, Jeong MH, Shin JH, Joo SB, Kim W, Lee SU, Kim KH, Kim NH, Cho JH, Park JC, Na KJ, Ahn YK, Cho JG, Ahn BH, Park JC, Kang JC. The role of chronic infection and inflammation in Korean patients with coronary artery disease. Korean Circ J 2000. 30:1107ŌĆō1116.

17. Ness J, Aronow WS. Prevalence of coronary artery disease, ischemic stroke, peripheral arterial disease, and coronary revascularization in older African Americans, Asians, Hispanics, whites, men, and women. Am J Cardiol 1999. 84:932ŌĆō933A7PMID : 10532515.


18. Lee DH. Infection and treatment of Helicobacter pylori in Korea. Korean J Gastroenterol 2002. 39:153ŌĆō160.
19. Strachan DP, Mendall MA, Carrington D, Butland BK, Yarnell JW, Sweetnam PM, Elwood PC. Relation of Helicobacter pylori infection to 13 year mortality and incident ischemic heart disease in the Caerphilly Prospective Heart Disease Study. Circulation 1998. 98:1286ŌĆō1290PMID : 9751676.


20. Thom DH, Grayston JT, Siscovick DS, Wang SP, Weiss NS, Daling JR. Association of prior infection with Chlamydia pneumoniae and angiographically demonstrated coronary artery disease. JAMA 1992. 268:68ŌĆō72PMID : 1608116.


21. Seong IW, Jeon ES, Choe SC. Meaning of serum antibody to Chlamydia pneumoniae in patients with restenosis after coronary balloon angioplasty or stent insertion. Korean Circ J 2001. 31:398ŌĆō404.

22. Zhou YF, Leon MB, Waclawiw MA, Popma JJ, Yu ZX, Finkel T, Epstein SE. Association between prior cytomegalovirus infection and the risk of restenosis after coronary atherectomy. N Engl J Med 1996. 335:624ŌĆō630PMID : 8687516.


23. Megraud F. Epidemiology of Helicobacter pylori infection. Gastroenterol Clin North Am 1993. 22:73ŌĆō88PMID : 8449572.


24. Nilsson PM, Moller L, Ostergren PO. Social class and cardiovascular disease-an update. Scand J Soc Med 1995. 23:3ŌĆō8PMID : 7784850.


25. Patel P, Mendall MA, Carrington D, Strachan DP, Leatham E, Molineaux N, Levy J, Blackston C, Seymour CA, Camm AJ. Association of Helicobacter pylori and Chlamydia pneumoniae infections with coronary heart disease and cardiovascular risk factors. BMJ 1995. 311:711ŌĆō714PMID : 7549683.



26. Murray LJ, Bamford KB, O'Reily DP, McCrum EE, Evans AF. Helicobacter pylori infection: relation with cardiovascular risk factors, ischaemic heart disease, and social class. Br Heart J 1995. 74:497ŌĆō501PMID : 8562233.



27. Niemela S, Karttunen T, Korhonen T, Laara E, Karttunen R, Ikaheimo M, Kesaniemi YA. Could Helicobacter pylori infection increase the risk of coronary heart disease by modifying serum lipid concentrations? Heart 1996. 75:573ŌĆō575PMID : 8697159.



28. Oshima T, Ozono R, Yano Y, Oishi Y, Teragawa H, Higashi Y, Yoshizumi M, Kambe M. Association of Helicobacter pylori infection with systemic inflammation and endothelial dysfunction in healthy male subjects. J Am Coll Cardiol 2005. 45:1219ŌĆō1222PMID : 15837252.


29. Han JY, Park JS, Yu KH, Choi YJ, Chae IH, Kim HS, Son DW, Oh BH, Lee MM, Park YB, Choi YS, Lee YW. The effects of Helicobacter pylori and cytomegalovirus infection on the risk of restenosis after percutaneous transluminal coronary angioplasty. Korean Circ J 2000. 30:39ŌĆō48.

30. Kowalski M, Konturek PC, Pieniazek P, Karczewska E, Kluczka A, Grove R, Kranig W, Nasseri R, Thale J, Hahn EG, Konturek SJ. Prevalence of Helicobacter pylori infection in coronary artery disease and effect of its eradication on coronary lumen reduction after percutaneous coronary angioplasty. Dig Liver Dis 2001. 33:222ŌĆō229PMID : 11407666.


Figure┬Ā1
There was no significant difference between the normal control group and the CAD group. NS, non-significant; H. pylori, Helicobacter pylori; CAD, coronary artery disease.
Table┬Ā1
Comparison of the demographics and coronary risk factors of the normal control group and the coronary artery disease group
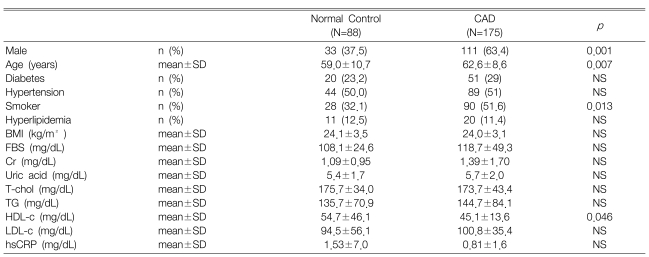
p, p-value; NS, non-significant; CAD, coronary artery disease; BMI, body mass index; FBS, fasting blood sugar; Cr, creatinine; T-chol, total cholesterol; TG, triglyceride; HDL-c, high density lipoprotein cholesterol; LDL-c, low density lipoprotein cholesterol; hsCRP, Highly sensitive C-reactive protein; SD, standard deviation
-
METRICS

- Related articles
-
Association between thyroid autoimmunity and Helicobacter pylori infection2017 March;32(2)



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print


